Transforming Mental Health Billing Challenges into Solutions
Recognitions & Certificates of Compliance

ASP-RCM Solutions - Billing Solutions For Your Mental Health Practice
Payer Guidelines are constantly evolving, we are here for your Mental Health billing codes, payer policies, Fee Schedule reimbursements, ensuring you make remarkable changes in your patient lives.
Meritoriously steering these changes requires Mental Practices to continuously stay current on new payer changes, state coverage directives and more.
By partnering with ASP-RCM, you gain access to Mental Health industry expertise, while your Physicians and Clinicians focus on changing this world better for Behavioral issues patients.
RCM Solutions for Varied Therapies

- Major Depressive Disorder
- Generalized Anxiety Disorder
- Bipolar Disorder
- Schizophrenia
- Post-Traumatic Stress Disorder
- Obsessive-Compulsive Disorder
- Borderline Personality Disorder
- Substance Use Disorder
- Alzheimer's Disease
- Intellectual and developmental disabilities
- Occupational Therapy
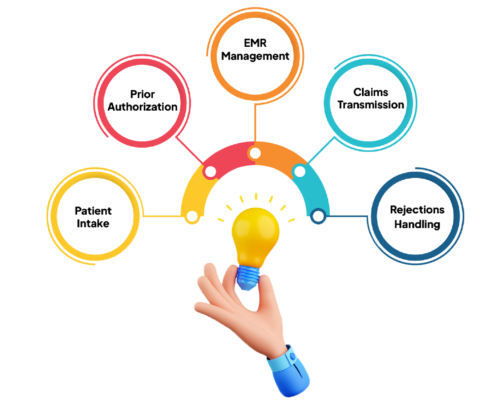
Mental Health Pre-Billing Process Includes

- Patient Intake
- Benefit Verification
- Prior Authorization
- EMR Management – Charge review
- Claims Transmission
- Rejection Handling
- Our certified billers understand how to handle Patient Intake & Prior Authorization to ensure that the entire treatment plan hours being authorized.
- We understand the dynamics on major payer requirements on Prior auth, ensuring that we submit the medical documentation for Auth approval
- Our efficient billing and claims transmission process results in a first-pass success rate of 85 percent, thus improving your reimbursement percentage significantly.
To Begin Enhancing your Revenue Cycle Management, Schedule a Consultation. Start Now!
Our Payment Reconciliation process includes

- ERA/EOB Posting
- Cash Posting & Self Pay Posting
- Denial Capture & Tracking
- Payment Reconciliation with Bank Deposits
- Flag Under or over payment
- Patient Invoicing
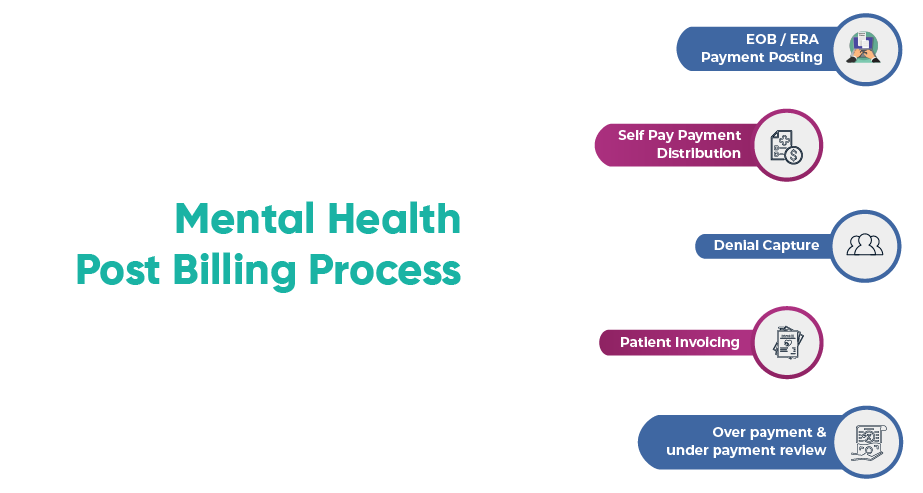
If you are Struggling to invoice Mental Health & ABA clients on patient responsibility – we can help streamline your process
Our Payment Reconciliation Process provides complete visibility on the payments received from Insurance and Patients. We post & reconcile these payments through ERA or Manual EOB and ensure that the patient account zeroed out.
Out of Pocket or Balance billing being monitored, tracked and updated to patient portal for patient reimbursements.
Our patient coordinators handle any queries from patients on their statements ensuring that we provide 360 degree easy experience for our clients and patients.
Accelerate your Collections with our Post Bill Process on One Touch Resolution Process
Do you want to avoid writing off claims as bad debt or non collectable – call us to know our AR strategy and Accelerate your collections
Our Collectors are not just callers, they are analyst, who understand the dynamics of Payer changes. Our experienced team of specialist will ensure that they address every single claim that have not been paid.
Our Process Excellence Team will also find the root causes for these unpaid or denials and provide process engineering strategies for Pre-Bill Process.
This ensures that a constant cycle of continuous excellence evolves throughout our client partnership.

To Begin Enhancing your Revenue Cycle Management, Schedule a Consultation. Start Now!