Your Therapy, Our ABA Billing Service Seamless Integration
Medical Billing Solutions For Your ABA Practice - ASPRCM Solutions
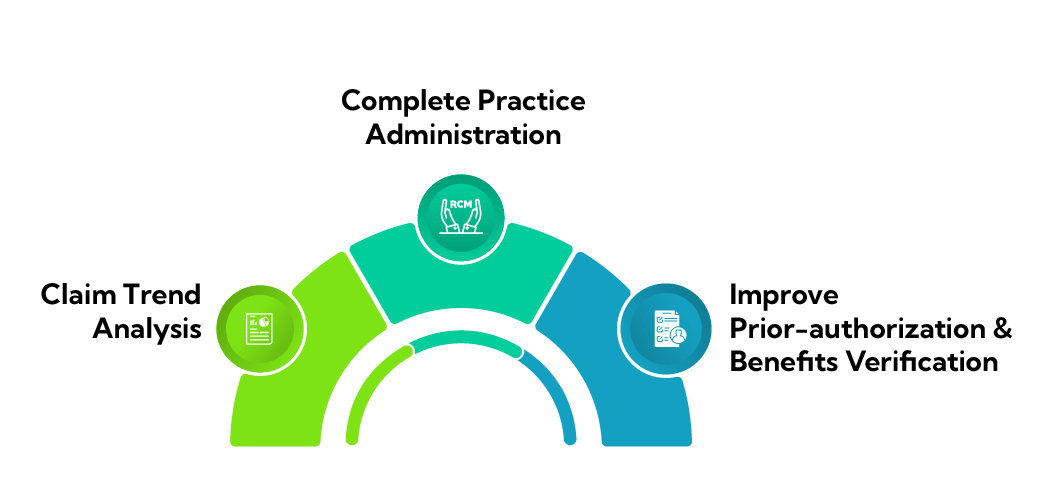
For ABA therapists to stay current on payer policies, billing requirements, and fee schedule reimbursements, ASP-RCM Solutions provides a unique set of billing features. We recognize that complying with payer restrictions and market advancements might be difficult for ABA therapy. To ensure that practitioners can significantly enhance patient care, our team of professionals is committed to remaining up to date on Medicaid changes, copays, deductibles, and private insurance.
Partnering with ASP-RCM gives you access to industry knowledge in the mental health field. At the same time, your therapists and clinicians can work to improve the lives of patients with behavioral health difficulties.
Understanding and Tackling ABA Billing Complexities
- Insurance Complexity: Navigating insurance policies, obtaining authorizations, and understanding coverage limitations can be time-consuming.
- Authorization and Pre-approval: Obtaining prior authorization from insurance companies can disrupt continuity of care.
- Documentation Requirements: Comprehensive documentation, including treatment plans, progress reports, and challenges, is necessary.
- Timely Claims Submission: Prompt submission of claims to insurance companies is crucial.
- Regulatory Requirements: Staying informed about policies, guidelines, and requirements changes is crucial for compliance and financial stability.
- Rate Negotiation: Negotiating reimbursement rates with insurance companies can be complex.
- Staff Training and Education: Ongoing training for billing staff and ABA practitioners is necessary.
- Appeals Process: Understanding the appeals process and providing additional documentation is necessary.
- Technology Integration: Implementing and managing billing software and EHR systems can be challenging.
- Collaboration with ASP-RCM solutions can increase efficiency, reduce billing errors, and improve financial outcomes for ABA practices.
end to end aba billing services
RATE
SUCCESS RATE
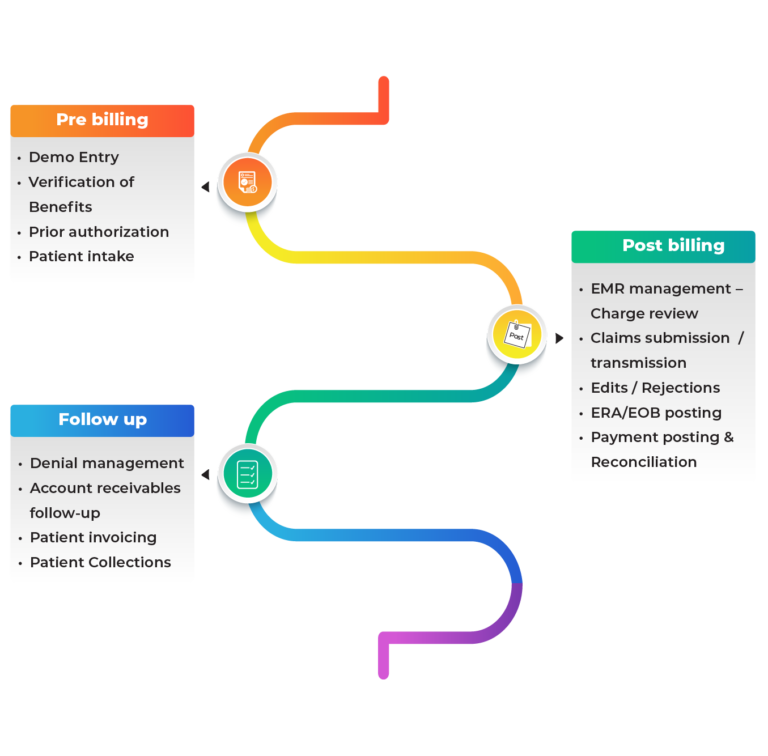
We provide end-to-end ABA billing services:
Our services cover the complete revenue cycle, from front-end to back-end, and include the following:
Pre Billing Process:
Before beginning any treatment plan or billing, we typically collect complete patient data, confirm insurance benefits, get prior authorization, and evaluate patient demographics.
Post Billing Process
Our billing staff verifies charges in the EMR system to ensure error-free invoicing. We submit claims to payers electronically, reply to any changes or denials, and then resubmit them for reprocessing. We also make insurers’ EOBs and ERA guidance available. Payments from insurance companies are posted to patient accounts and verified to be on the right account by comparing them to charges.
Follow Up Process
Our AR executives handle patient invoicing, patient collections, follow-up on accounts receivable, and denial management. We examine the reasons for denials, resolve issues, and resubmit claims. We prepare and mail bills for out-of-pocket expenses and support the ABA agency in collecting overdue sums.
How we can keep your ABA Clinics going
- Maximizing reimbursements through expert billing practices
- Utilizes specialized ABA billing services for higher reimbursement rates.
- Understand ABA-specific billing and payer policies for optimized claim values.
- Ensuring accuracy with clean claim submission
- Uses rigorous post-billing processes for clean claims submission.
- Reduces claim denials and rejections by ensuring claims meet insurance standards.
- Cost savings through efficient billing management
- Outsourcing billing to an expert team reduces operational costs and enhances revenue.
- In addition, receive comprehensive client portal support and a complimentary EMR consultation to elevate your therapy to a new level.
Medical Billing and Revenue Cycle Management for a Wide Variety of Medical Specialities
To Begin Enhancing your Revenue Cycle Management, Schedule a Consultation. Start Now!