You Take Care Of Your Patients. Let Us Handle The Benefit Verification Process
and revenue loss to a practice

Eligibility Verification and Benefits Check
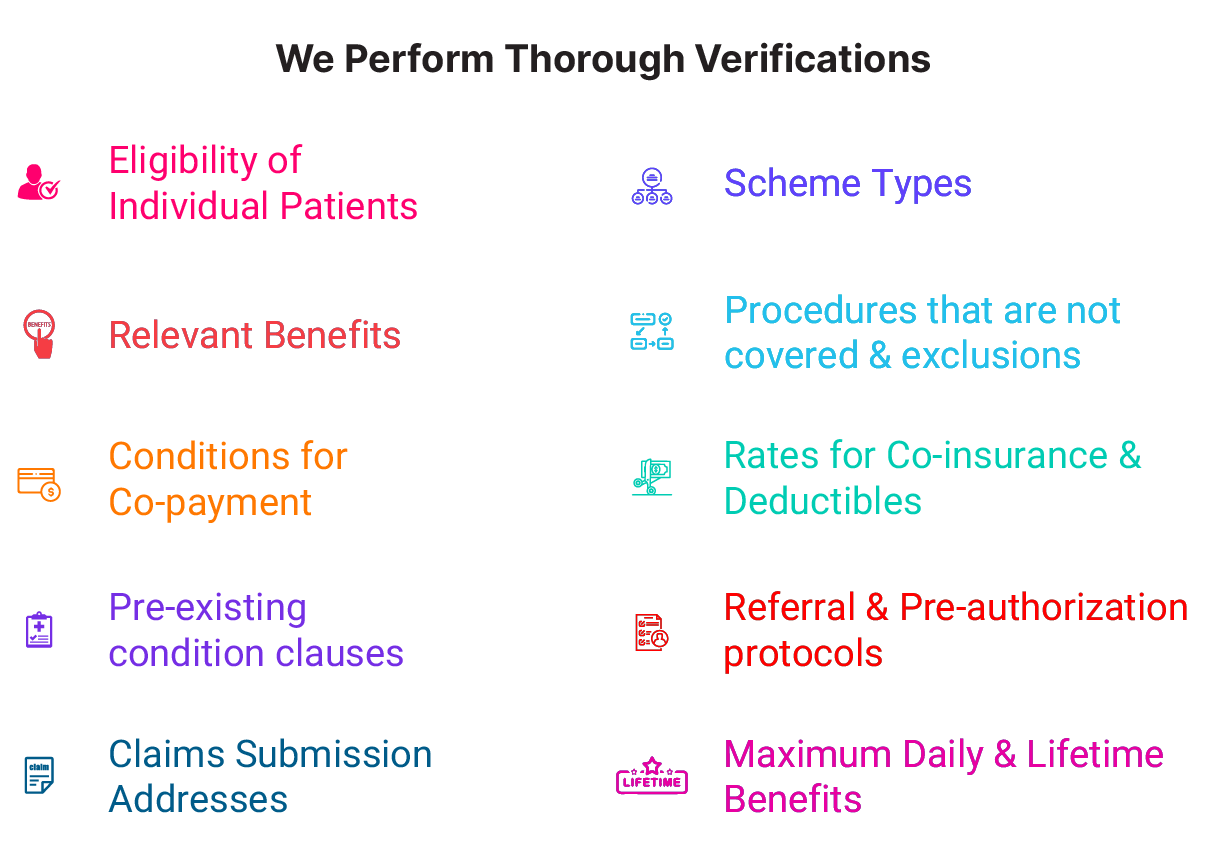
Our verification process looks at the coverage specifics of each procedure and any possible out-of-pocket costs. Patients can comprehend their financial responsibilities before their appointment because of this transparency. Patient payments are made on time, back-end collections are reduced, patient satisfaction is increased, and revenue generation is maximized.
Technical Aspects of Eligibility Verification and Benefits Check:

EDI Transactions: Utilizing Electronic Data Interchange (EDI) transactions, specifically the 270/271 transactions, healthcare providers can electronically inquire about a patient’s insurance eligibility and receive a response in real-time or batch mode. The 270 transaction is the inquiry, and the 271 transaction is the insurer’s response.
Integration with Practice Management Systems: Incorporating eligibility verification as an integral part of the practice management system allows for seamless workflow and reduces manual errors. This integration ensures that patient data is automatically pulled from the system for verification, and the results are populated back into the system.
Utilizing APIs for Real-time Verification: Application Programming Interfaces (APIs) can be employed to facilitate real-time insurance eligibility checks. APIs enable instantaneous data exchange and verification by connecting the healthcare provider’s system directly with the payers.
Data Standardization and Validation: Implementing data standardization and validation protocols ensures that the information sent for verification is accurate and formatted correctly, reducing the chances of errors and denials.
Automated Verification Tools: Leveraging automated verification tools can significantly reduce the turnaround time for eligibility checks. These tools can be programmed to conduct verification checks at predetermined times, such as during patient check-in or a day before the appointment.
Robust Reporting and Analytics: Having full reporting and analytics in place helps in tracking the effectiveness of the eligibility verification process. It provides insights into patterns of denials, joint issues, and areas that require attention, enabling practices to make data-driven decisions for process improvement.
To Begin Enhancing your Revenue Cycle Management, Schedule a Consultation. Start Now!