Benefits of Prior Authorization in ABA Therapy
Healthcare insurance companies utilize the prior authorization process to decide whether to pay for a specific medical treatment or procedure before it is carried out. Before beginning treatment, healthcare practitioners must receive authorization from the insurance provider. Prior Authorization is used to confirm that a treatment or operation is medically required and fits the requirements for the coverage set forth by the insurance provider.
An intervention used to treat people with autism spectrum disorder (ASD) and other developmental issues is called ABA therapy or Applied Behavior Analysis therapy. It is a methodical technique that concentrates on behavior analysis and modification to assist people in developing their social, communicative, and adaptive skills while lowering problematic behaviors.
Benefits of Prior Authorization in ABA Therapy
Ensuring that clients and providers have an easier time working with effective treatment methods:
Prior authorization is a good idea to verify that ABA therapy is medically essential for the patient receiving treatment. Based on the patient's diagnosis and particular behavioral problems, healthcare professionals must
produce paperwork and proof proving the need for ABA therapy.
Additionally, prior authorization enables insurance providers to evaluate the qualifications and experience of ABA therapy providers. Before approving a treatment, insurance companies may demand that the practitioner meet certain qualifications, certifications, or licensing standards. It encourages the employment of qualified professionals in the sector and works to protect the standard of care given to people with autism spectrum disorder (ASD).
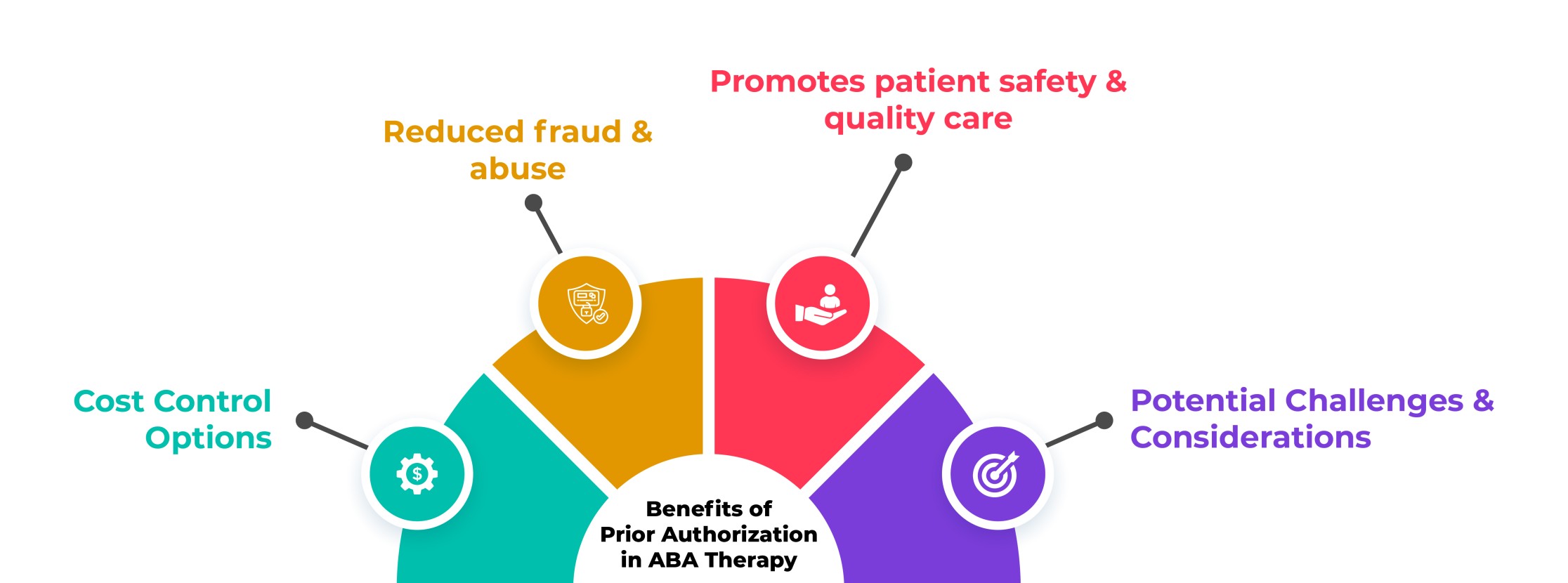
1. Cost Control Options
Prevents unnecessary or ineffective treatments: Prior authorization helps control healthcare costs by avoiding the coverage of unnecessary or ineffective ABA therapy treatments. Through the review process, insurance companies can assess the medical necessity and appropriateness of the requested treatment. This ensures that only medicines that have demonstrated efficacy in improving the individual's condition are approved for coverage. Insurance companies can allocate resources more efficiently and reduce unnecessary healthcare expenditures by avoiding unnecessary or ineffective treatments.
Encourages evidence-based practices: Prior authorization promotes the use of evidence-based practices in ABA therapy. Insurance companies typically require providers to submit documentation and treatment plans based on established research and best practices in the field. This requirement promotes the use of interventions that are effective in treating individuals with autism spectrum disorder (ASD). By prioritizing evidence-based practices, insurance companies can optimize the use of resources by supporting treatments that have a higher likelihood of positive outcomes and cost-effectiveness.
2. Reduced fraud and abuse.
Another benefit of prior authorization in ABA therapy is its role in reducing fraud and abuse within the healthcare system. Here's how it helps:
Detecting fraudulent claims: Prior authorization requires healthcare providers to submit documentation and information about the individual's diagnosis, treatment plan, and the qualifications of the ABA therapy providers. Insurance companies review these submissions to ensure the requested treatment is appropriate and necessary. This process helps detect discrepancies and Fraudulent Claims, such as submitting false information or exaggerating the need for treatment. By scrutinizing the details of the treatment request, insurance companies can identify and prevent fraudulent activities, protecting both the healthcare system and the individuals receiving ABA therapy.
Ensuring compliance with guidelines: Prior authorization involves evaluating the treatment request against specific criteria and guidelines set by the insurance company. These guidelines often include requirements related to the qualifications of providers, treatment duration, and other relevant factors. By enforcing these guidelines, insurance companies can prevent providers' abuse of resources, such as overbilling or excessive treatment sessions. Prior authorization is a safeguard to ensure that ABA therapy is provided within reasonable and appropriate parameters, reducing the potential for fraudulent practices.
3. Promotes patient safety and quality care.
Prior authorization in ABA therapy also plays a role in promoting patient safety and ensuring the delivery of quality care. Here's how it contributes to these important aspects:
Assessing provider qualifications: Prior authorization requires healthcare providers to meet specific qualifications and credentials set by the insurance company. This evaluation process helps ensure that individuals receive ABA therapy from qualified professionals with the necessary training and expertise to deliver safe and effective care. By verifying provider qualifications, prior authorization promotes patient safety by reducing the risk of receiving treatment from unqualified or inexperienced practitioners.
Reviewing treatment plans: Prior authorization involves a review of the proposed ABA therapy treatment plans. This review process allows insurance companies to assess the appropriateness of the treatment approach, ensuring that it aligns with evidence-based practices and the specific needs of the individual. By scrutinizing treatment plans, prior authorization helps identify potential risks or gaps in care, promoting patient safety and ensuring that the therapy is tailored to the individual's unique requirements.
Monitoring treatment outcomes: Prior authorization may include a monitoring component, where insurance companies assess the progress and results of the ABA therapy over time. This helps ensure that the treatment remains effective and beneficial for the individual. By monitoring treatment outcomes, prior authorization contributes to quality care by identifying any necessary adjustments or modifications to the treatment plan, promoting continuous improvement and positive results for the patient.
4. Potential Challenges and Considerations
Implementing Prior Authorization in ABA therapy can come with certain challenges and considerations. Here are a few potential ones to keep in mind:
Delayed access to treatment: The prior authorization process can introduce delays in accessing ABA therapy. The review and approval process may take time, impacting individuals who require timely intervention. Administrative burden: Prior authorization can impose additional administrative tasks on healthcare providers, requiring them to gather and submit documentation, treatment plans, and other necessary information to insurance companies.
Varied insurance requirements: Different insurance companies may have varying requirements for prior authorization in ABA therapy.
Determining medical necessity: Assessing and determining medical conditions can be subjective and vary between insurance companies and healthcare providers. This can lead to disagreements and challenges in obtaining prior authorization.
Adequate coverage and reimbursement: Prior authorization should not result in limited coverage or inadequate reimbursement for ABA therapy. It is important to ensure that insurance companies provide a reasonable range of necessary and evidence-based ABA therapy services.
Conclusion
Prior authorization in ABA therapy, combined with the implementation of ASP-RCM solutions, can further enhance the benefits and address the challenges associated with this process. ASP-RCM Solutions provide technological tools and software that streamline the prior authorization process, improve efficiency, and reduce administrative burdens. These solutions automate documentation submission, facilitate communication between healthcare providers and insurance companies, and offer real-time tracking and status updates.




