BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Elevate your Durable Medical Equipment (DME) business with our specialized DME Billing Services
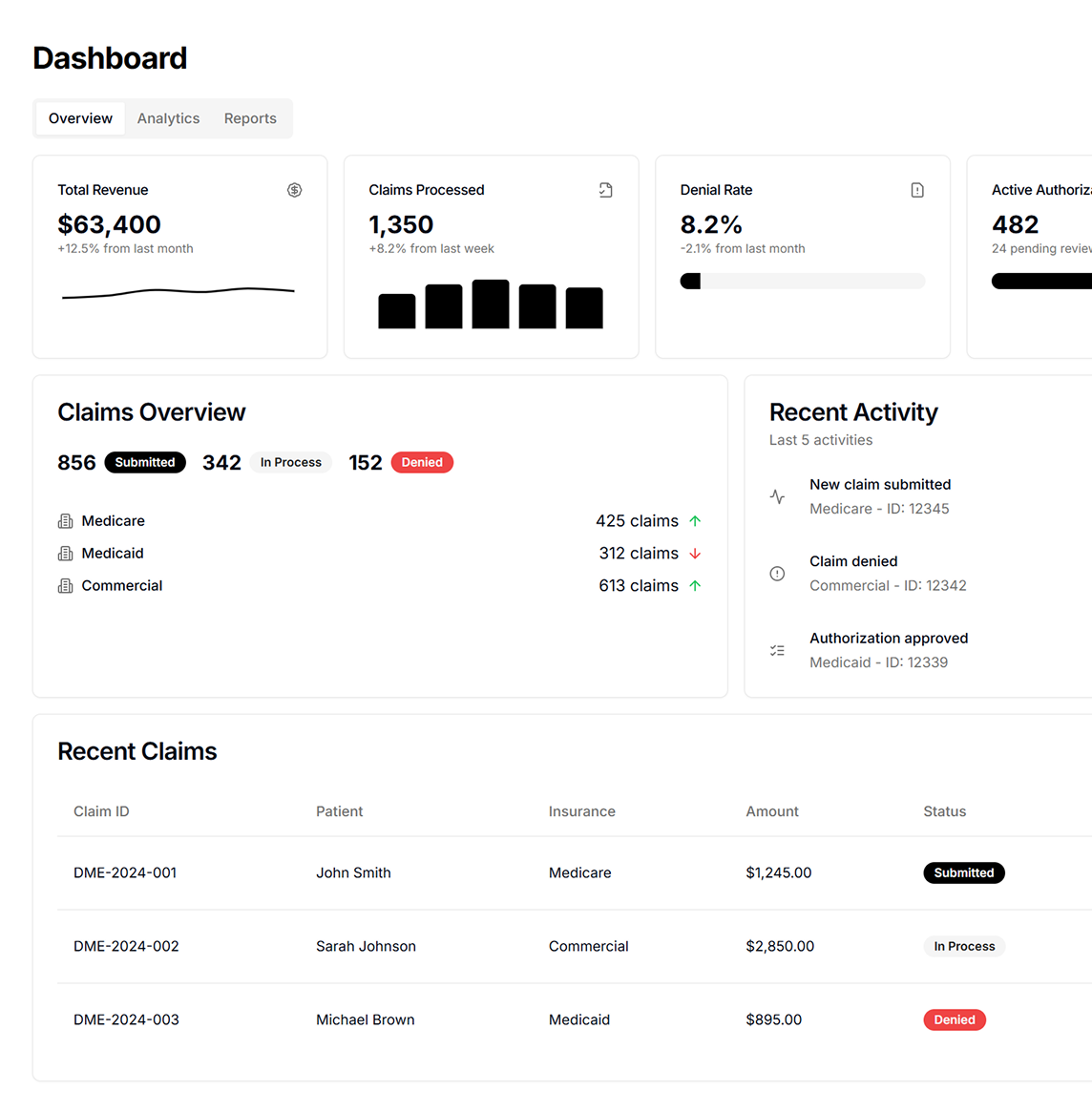
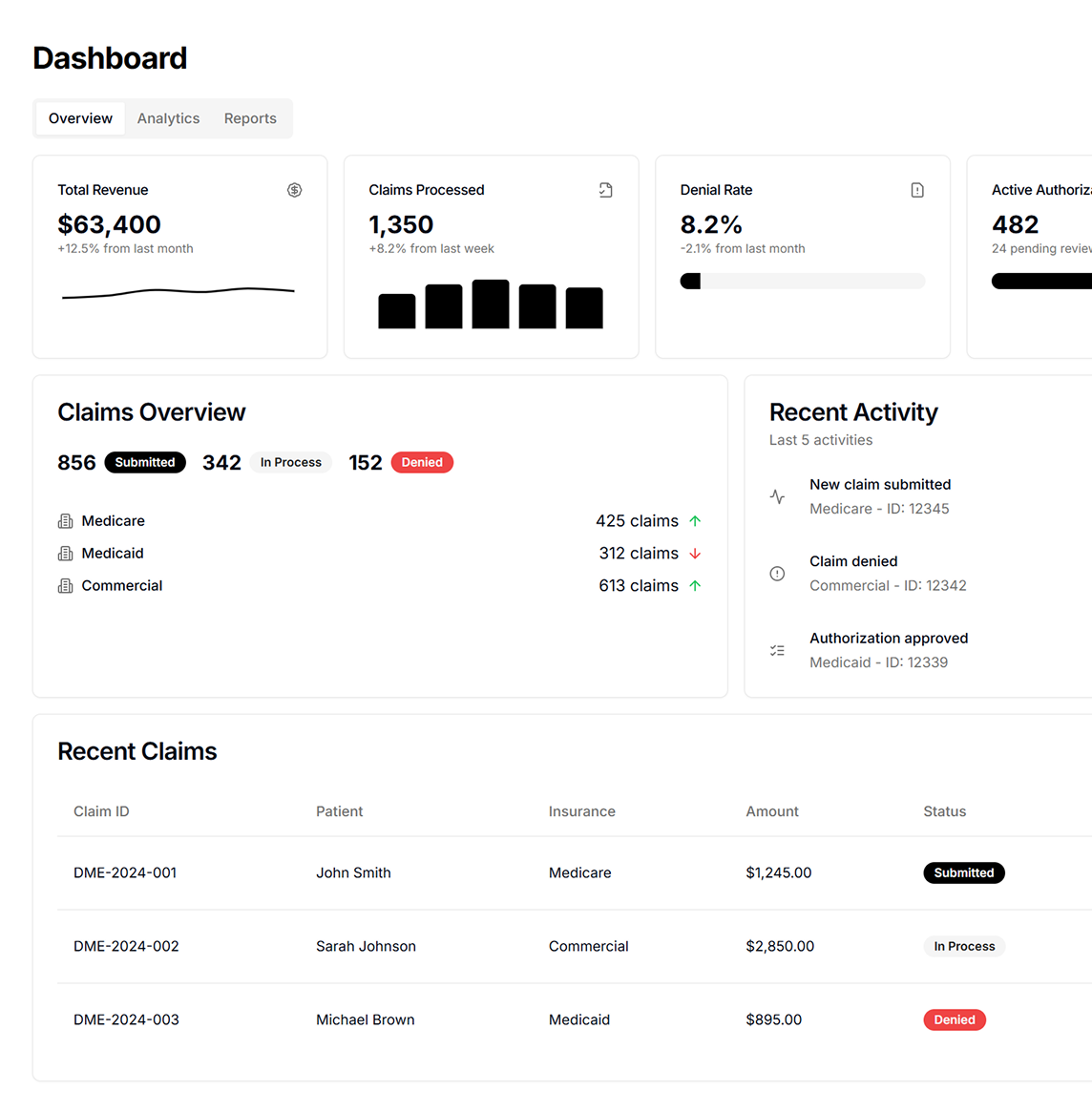
Schedule a CallTotal Claims Processed
Total Revenue Billed
Denial Rate
By fusing technology with expertise, we offer a powerful billing platform that scales with your practice, remains vigilant on regulatory mandates, and continues to innovate for better profitability
• Eligibility Verification & Prior Authorization of products • Patient Demographics Entry and Order Entry • HCPCS Level II Coding & Modifiers • Claims Submission to payers • Payment Posting & Reconciliation • Accounts Receivable & Denial Management • Credit Balance Resolution
• 97% Net Collection Rate – We help practices recover the maximum possible revenue • 35 Days AR Reduction – Our efficient processes shorten the time claims spend in Accounts Receivable • Lower Denial Trends – Thorough claim scrubbing and appeals lead to industry‑low denial rates • Seasoned in Rental Order Billing – Expertise in complex rental billing scenarios for DME item
Our refined workflows address every phase of DME billing to increase speed and accuracy: • Comprehensive Order Entry • Preauthorize Your Orders • Streamlined One‑Touch Claims • Payment Posting Reconciliation
• AI-Driven RCM: Real-time AR assessments with dynamic queues for denials, resolutions, and appeals • Automated Patient Invoicing: Streamlines payments, reducing confusion and accelerating collections • Customer Support: Patient coordinators enhance satisfaction with DME solutions
ASP‑RCM’s Analytics and Dashboards provide on‑demand reports covering billing performance, inventory levels, shrinkage, AR timelines, and more. Our insights empower your team to make data‑driven decisions that optimize both revenue acceleration and patient care quality
Is your top goal reducing bad debt and uncollectible claims? Our structured Accounts Receivable strategy identifies and rectifies denials promptly maximizing your net collections and keeping your revenue cycle healthy
We ensure strict adherence to CMS mandates and employ automated workflow tools that minimize paperwork delays, ensuring a quick transition from product dispensing to billing
Through electronic prior authorization, we verify coverage requirements before dispensing DMEPOS items. This proactive approach prevents billing setbacks and ensures suppliers meet all compliance rules pre‑delivery
By uniting automated and manual cash posting with daily deposits, we provide transparent reconciliation for each transaction. This reduces errors, accelerates revenue posting, and boosts financial clarity
Our AI‑based modules offer real‑time AR assessments, dynamically routing claims for resolution or appeal. This cuts down on denial backlogs and keeps your revenue cycle healthy and moving

From automated invoicing to dedicated patient coordinators, we prioritize clarity and ease. Patients benefit from simplified billing statements, while our support teams promptly resolve queries—bolstering satisfaction and payment compliance
ASP‑RCM’s advanced analytics dashboards deliver 360‑degree visibility into billing metrics, inventory control, AR performance, and patient experience metrics. This holistic oversight drives continuous process improvement and revenue optimization
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers