BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
By bridging the gap between accurate charge entries and audits, we elevate your billing processes to new heights, ensuring a healthier bottom line for your practice
Schedule a CallError Detection Rate
Claim Correction Rate
Compliance Adherence


Laying the Groundwork for Efficient Medical Billing
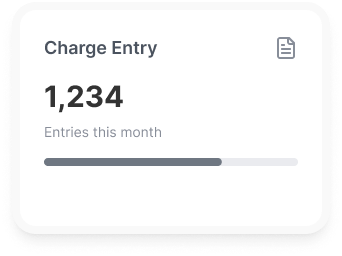
Our team inputs charges into your EMR or practice management system with a focus on accuracy and compliance. By following payer rules and clinic-specific guidelines, we ensure error-free charge entry, paving the way for successful claim submissions
We adopt a proactive strategy to handle clearinghouse rejections. Claims requiring additional documentation are held or pended for clarification, while our team ensures prior authorization numbers are verified and accurately included
We submit claims within one business day to minimize delays and keep your cash flow steady
Our team reviews daily appointment rosters to identify no-shows and discrepancies, ensuring that all billable services are accurately captured and submitted
We deliver detailed daily reports covering revenue billed, rejections resolved, and claims transmitted, giving you complete visibility into your billing performance and results
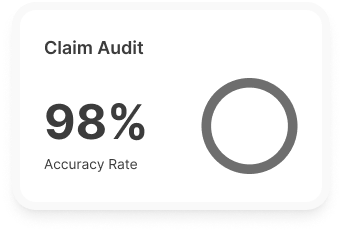
From verifying patient information to auditing claims for compliance with payer-specific rules
Our in-person collection oversight services ensure that front-desk staff effectively manage patient payments at the time of service. From copays to outstanding balances, we provide training, tools, and real-time support to streamline the collection process
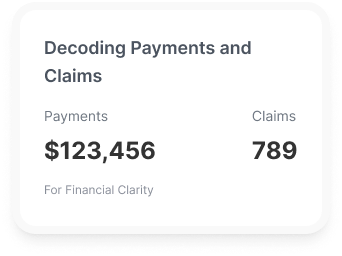
We simplify the often-confusing reconciliation process of EOBs and ERAs by ensuring that payments and adjustments align with what was billed. Our team reviews payer remittances thoroughly to identify underpayments, overpayments, and discrepancies, taking corrective actions where necessary
Denials don’t have to mean lost revenue. We specialize in analyzing denial trends and generating detailed reports on specific denial types. These insights allow your team to identify root causes, such as coding errors or authorization lapses, and implement strategies to prevent future occurrences

Our denial management services focus on recovering revenue from denied claims by addressing their causes head-on. From resubmitting claims with corrected information to engaging in payer negotiations, we make sure no claim is left unresolved
With rising out-of-pocket costs, managing patient liability has never been more important. We assist in calculating patient balances and implementing clear communication strategies to explain their financial responsibilities

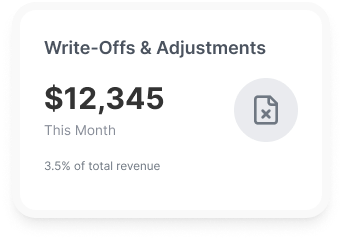
Write-offs and adjustments are an inevitable part of revenue cycle management, but they need to be handled carefully to maintain financial accuracy. We review each case meticulously to ensure adjustments are valid and compliant with payer contracts
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers