BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Our home health billing solutions experience the confluence of efficiency and empathy.
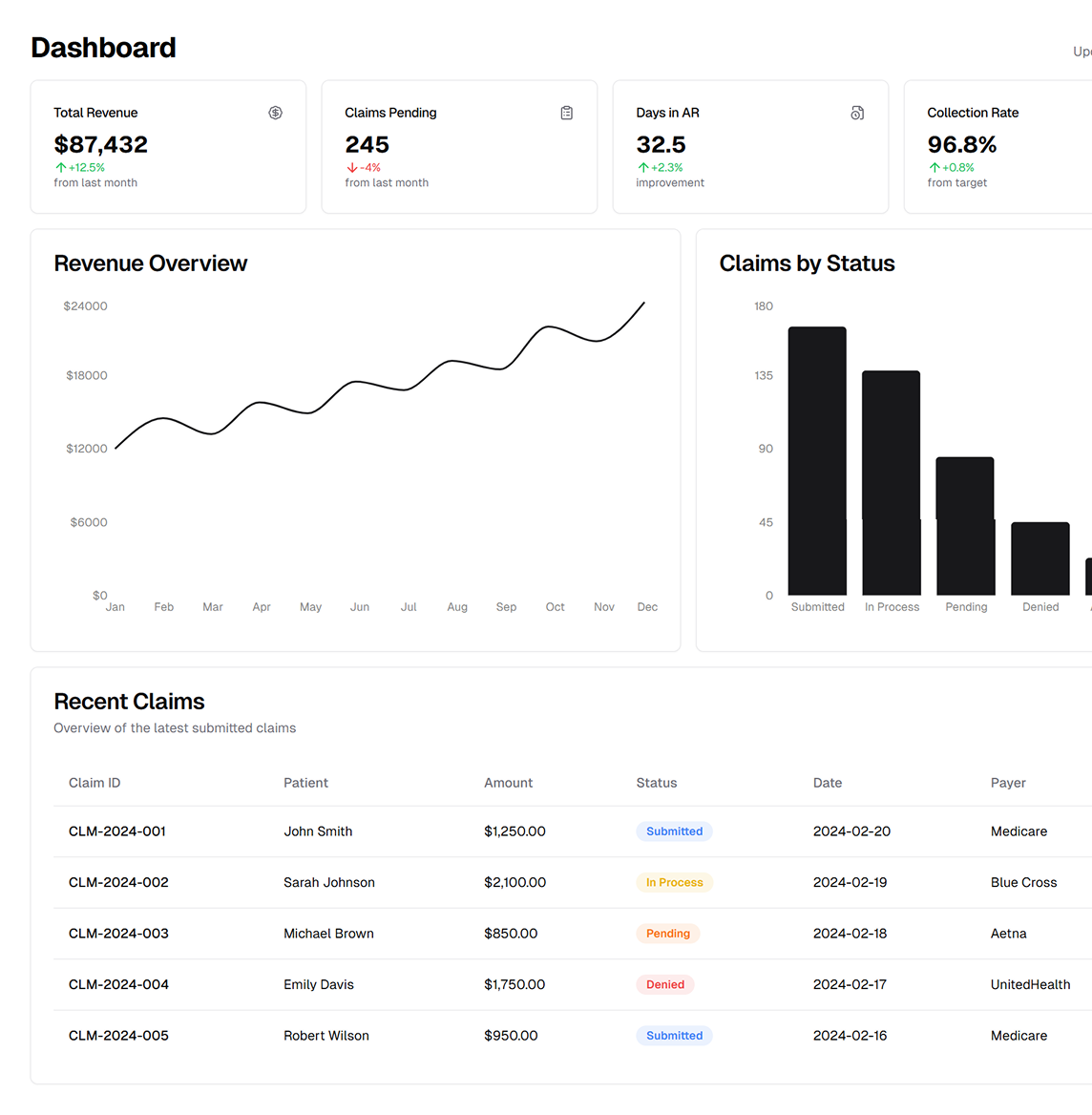
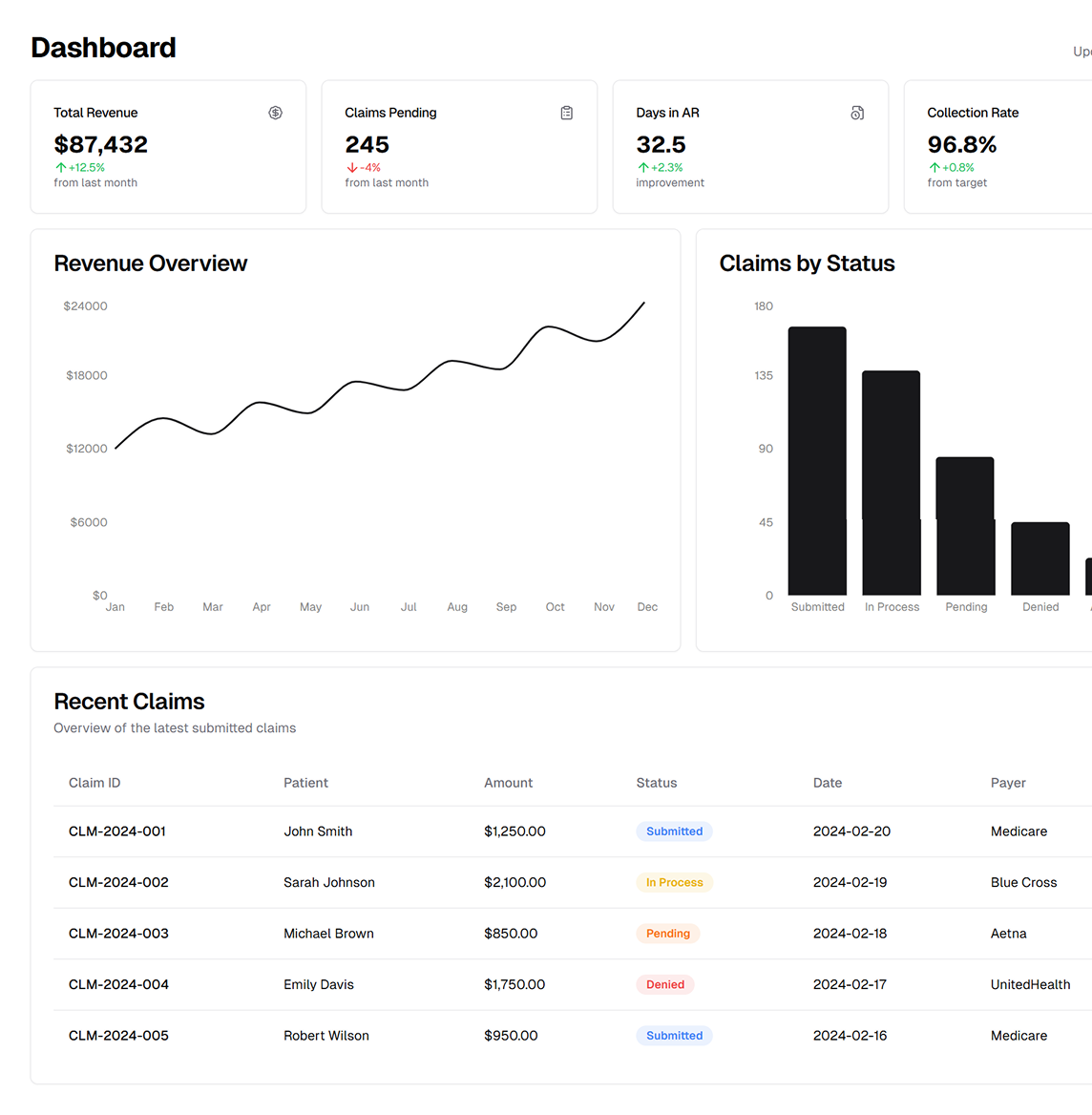
Schedule a CallTotal Visits Billed
Medicare Claim Denial Rate
Total Claims Submitted
ASP‑RCM Solutions customizes home care billing for Medicare, Medicaid, and private payers—tailored to your agency’s unique workflows. Trust our certified experts for complex coding (ICD‑10, PDGM, OASIS) and HIPAA compliance, ensuring accurate claims and optimal reimbursements.
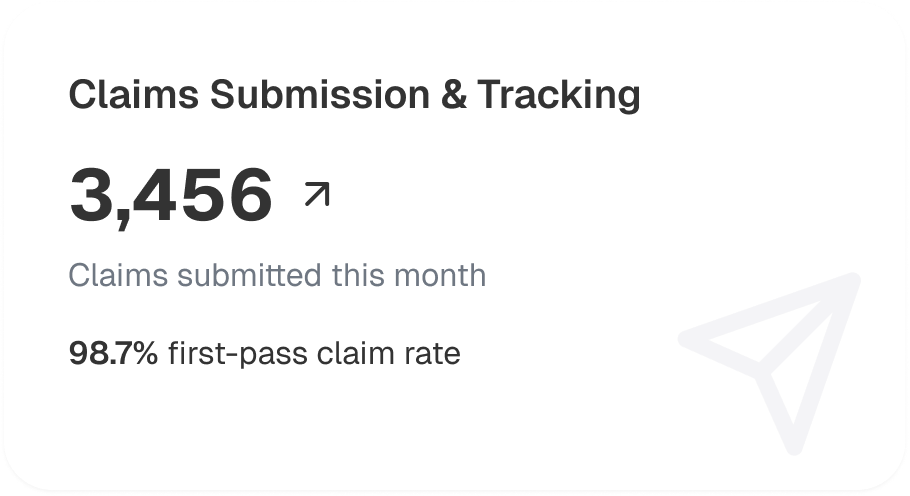
By collaborating with ASP‑RCM, agencies can expect to: • Increase Revenue by up to 12% through optimized coding and fewer claim rejections. • Get Paid Faster (up to 33% improvement) via efficient RCM workflows and electronic claims. • Reduce Overhead by ~5% with streamlined operations and minimized manual entries.
With years of experience in PDGM billing, we support a wide range of billing formats, including: • HCFA 1500, UB‑04, and HIPAA‑compliant electronic 837I or 837P submissions. • Fee‑For‑Service entry and consolidated data reporting. • Compliance with Medicare, Medicaid, HMOs, and private pay guidelines. • We ensure timely payment, accurate statistics, and thorough analysis of your home health agency billing
• Insurance Verification for coverage and co-pays. • Billing Analysis for PDGM and OASIS. • AR Aftercare for overdue/denied claims. • Denial Analysis for coding gaps. • Credentialing for payment compliance.
• 20% fewer denials with proactive coding. • Reduced errors, improved RCM efficiency. • Refunds & payments boost cash flow. • Tailored solutions with dedicated support. • Advanced tech for accurate coding & analytics. • Scalable services for growth.
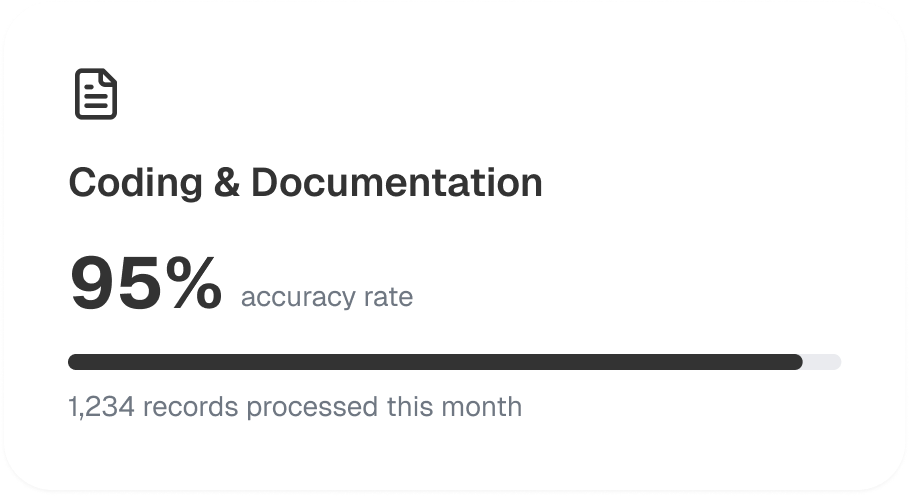
Our processes are designed around: • HIPAA & PHI security. • Coding audits, ICD-10 & PDGM updates. • Clean claims. • OASIS data integration for accurate billing.
Our operational framework covers everything from initial eligibility checks to final claim settlement, ensuring you remain compliant and profitable. We combine advanced technology with specialized home health expertise to deliver consistent results and adaptability in an ever‑changing reimbursement landscape.
We verify insurance coverage and benefits for new home health admissions, ensuring accurate payer information and reducing claim rejections later in the process

Certified home health coders proficient in ICD‑10, HCPCS codes, and PDGM guidelines meticulously document each patient encounter, enhancing claim accuracy and timeliness
We submit claims electronically using 837I/837P or UB‑04 as required, then track their progress. Our system flags any denial trends, enabling swift resolutions and fewer payment delays
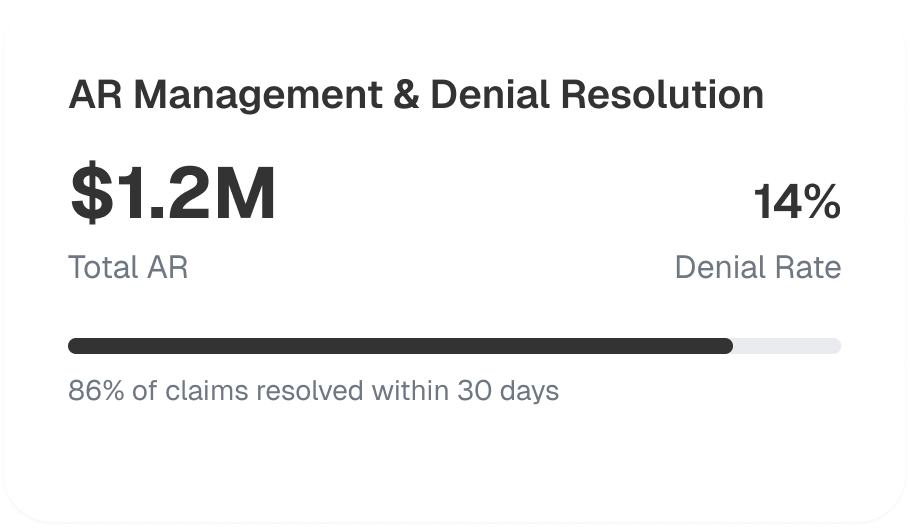
Our AR aftercare teams aggressively follow up on overdue or underpaid claims, analyzing common denial causes to refine coding and documentation, further decreasing front‑end denials
We ensure correct posting of all insurer and patient payments, reconciling accounts in real time. Any overpayments or adjustments are quickly processed to maintain positive cash flow

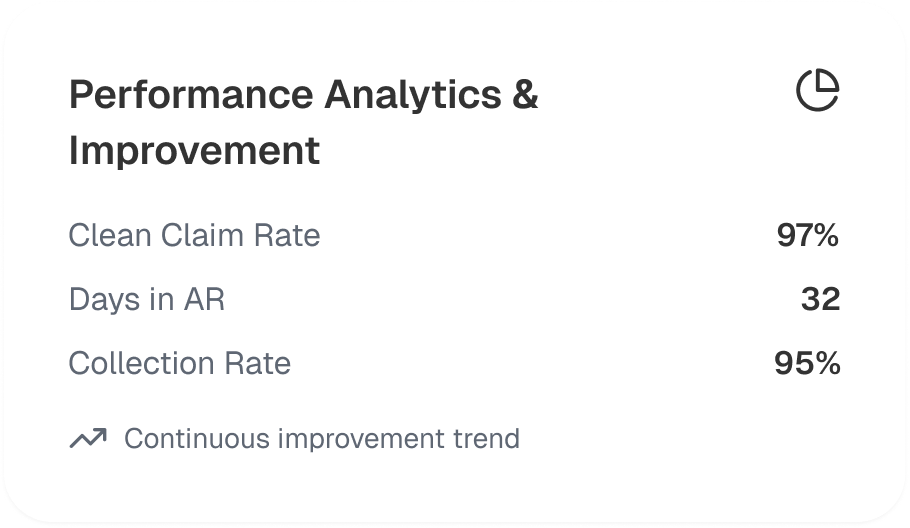
We generate detailed RCM and billing reports, highlighting metrics like clean claim rate, denial percentage, and days in AR. By analyzing these insights, we make iterative improvements to your home health billing process and keep you ahead of evolving industry regulations
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers