BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
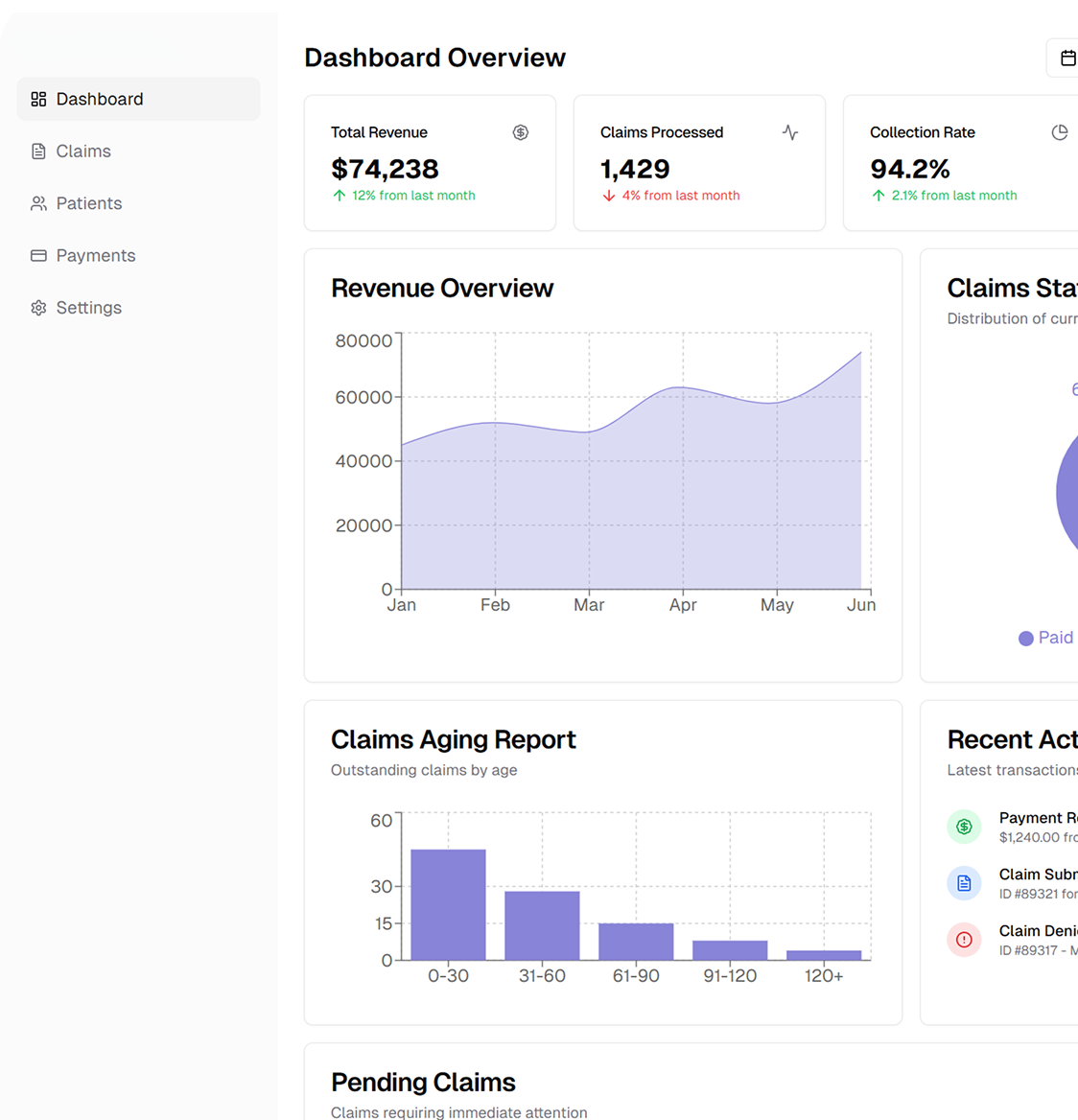
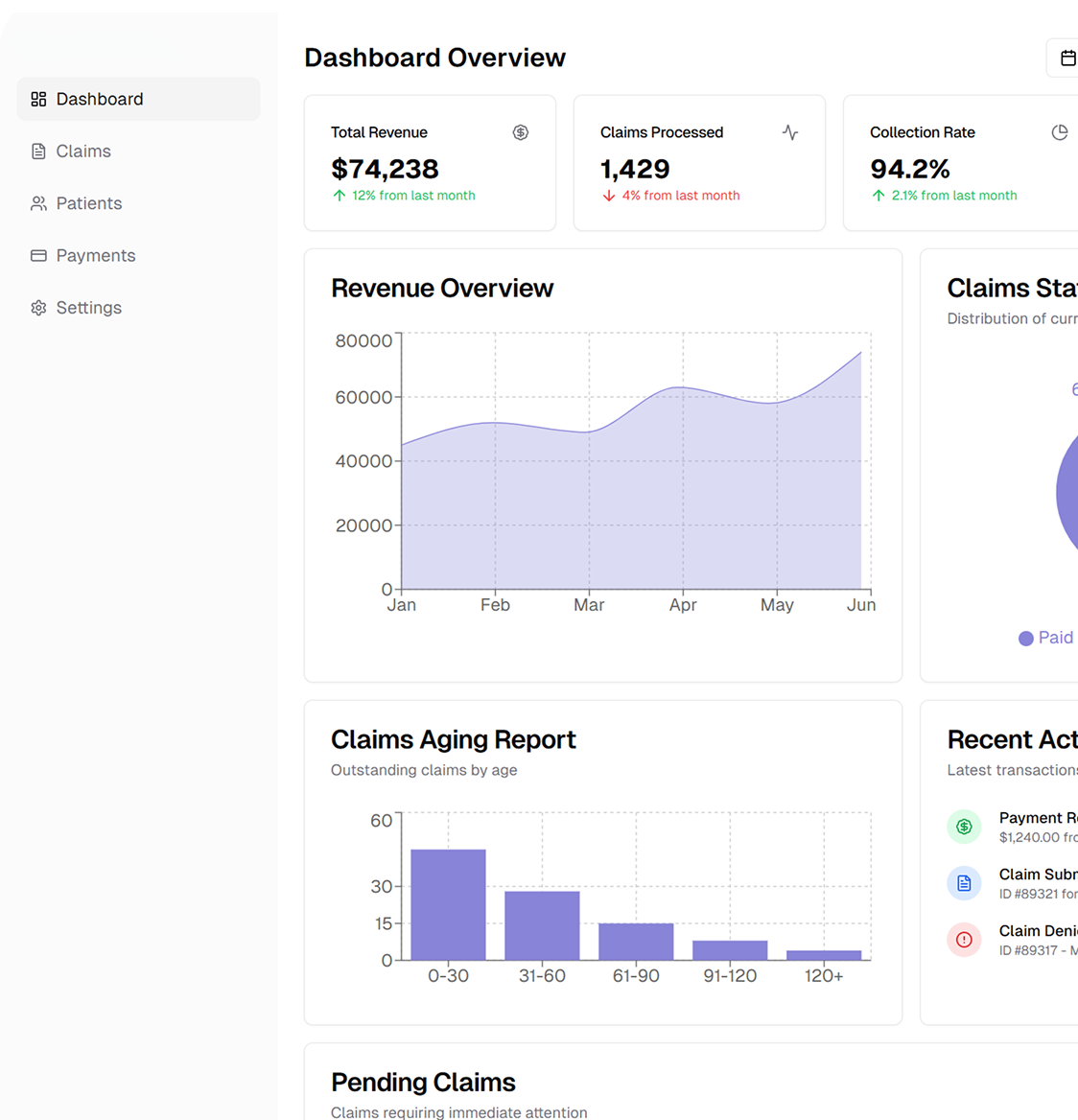
Our customized RCM services address billing challenges from patient registration to final payment - improving cash flow and minimizing administrative burdens
Schedule a CallAvg Time to Insurance Payment
Medical Necessity Denial Rate
Total Charges Submitted
Cardiology billing presents unique hurdles due to high‑cost treatments, frequent insurance authorizations, and ever‑evolving payer rules. Advances in cardiovascular care—from interventional cardiology to hybrid procedures—have introduced more intricate ICD‑10, CPT, and HCPCS coding requirements
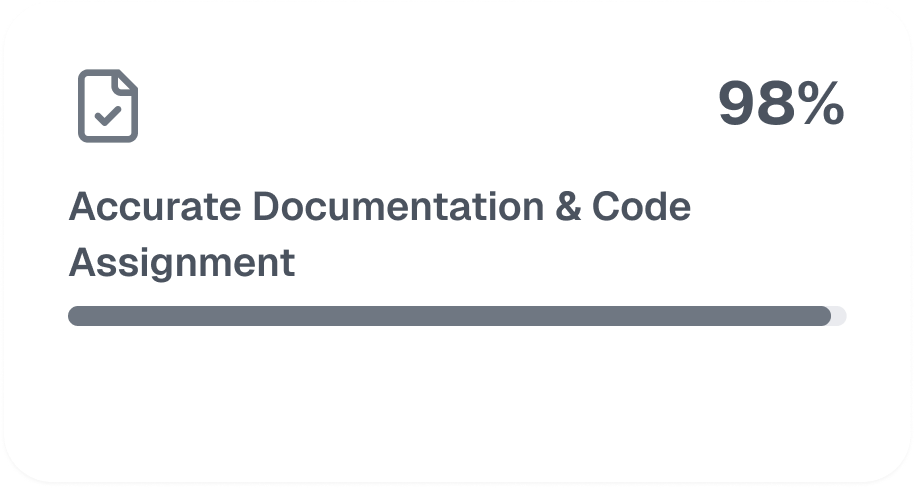
Our certified coders specialize in the complex differences between congenital and noncongenital cardiac procedures. We manage specific modifiers (e.g., -59, -51, -RT, -LT) and handle diagnostic locations (e.g., cath lab vs. outpatient) to ensure precise billing. Through super bill customization, we capture every payable service accurately, whether it’s CABG, PCI, EP testing, or device implants
• Effective cardiac medical billing starts with meticulous front‑end processes: • Insurance Verification: Collect and validate all coverage details upon scheduling. • Diagnostic Inclusion: List all relevant tests or labs when referring patients. • Payer Criteria: Check pre‑certification rules for high‑value or interventional procedures. • Authorizations: Confirm referral requirements and approvals before the visit. • By addressing these elements proactively, you minimize claim denials and protect your revenue stream.
We streamline cardiology billing with expert coding, reduced denials, secure data management, custom charge capture, and reimbursement tracking
• Expert Coders: CMS & AMA-compliant coding • Nationwide Service: 21+ states covered • Seamless Integration: EHR-friendly workflow • Certified Accuracy: AAPC-certified team
• Higher Revenue: Capture all allowable charges • Less Admin: We handle billing & compliance • Flexible: Scales for any practice size • Stay Compliant: Up-to-date with coding changes
Our operational framework unites front‑end checks (insurance verifications, authorizations) with back‑end revenue cycle tasks (denial management, payment posting, compliance). By aligning each phase of the cardiology billing process, we help you maintain consistent cash flow and minimize high‑dollar claim rejections
We gather patient demographics, confirm policy specifics, and manage pre‑certification steps. This upfront diligence reduces unexpected denials and ensures smoother scheduling for complex cardiology procedures
Content –Our coding team verifies medical records against ICD‑10, CPT, and HCPCS guidelines, differentiating between congenital and noncongenital conditions. We capture all relevant modifiers, location codes, and procedure details to produce clean, first‑pass claims
We integrate EHR documentation into a custom cardiology super bill, then submit electronic claims securely via 837P/837I forms. This streamlined submission flow expedites payer processing and reduces the risk of front‑end rejections.
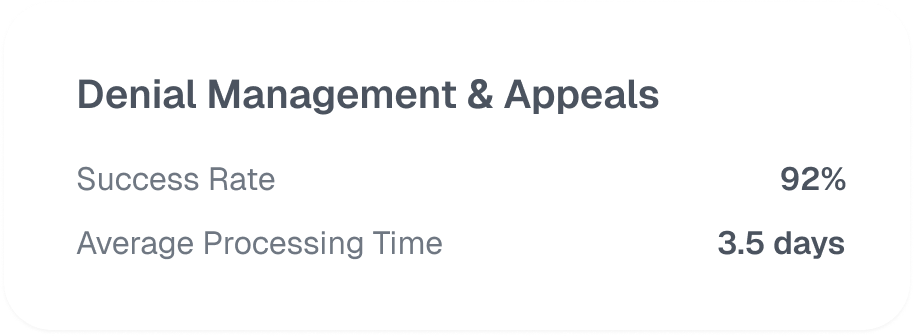
If rejections arise, our specialized denial team analyzes payer feedback, corrects any coding or documentation gaps, and files appeals promptly. By targeting high‑value cardiology claims first, we quickly stabilize your revenue stream
We use robust encryption and security protocols to safeguard patient information. Regular HIPAA audits and staff training maintain compliance, ensuring your cardiology practice meets all privacy standards
We provide monthly and quarterly performance dashboards, tracking metrics like denial rate, days in AR, and net reimbursement. These insights guide iterative enhancements, keeping your cardiology billing operations efficient and profitable

.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers