BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Our hospital billing solutions blend efficiency and empathy to optimize physician reimbursement and patient satisfaction
Schedule a CallTotal Revenue Billed
Avg Reimbursement Time
Claim Denial Rate
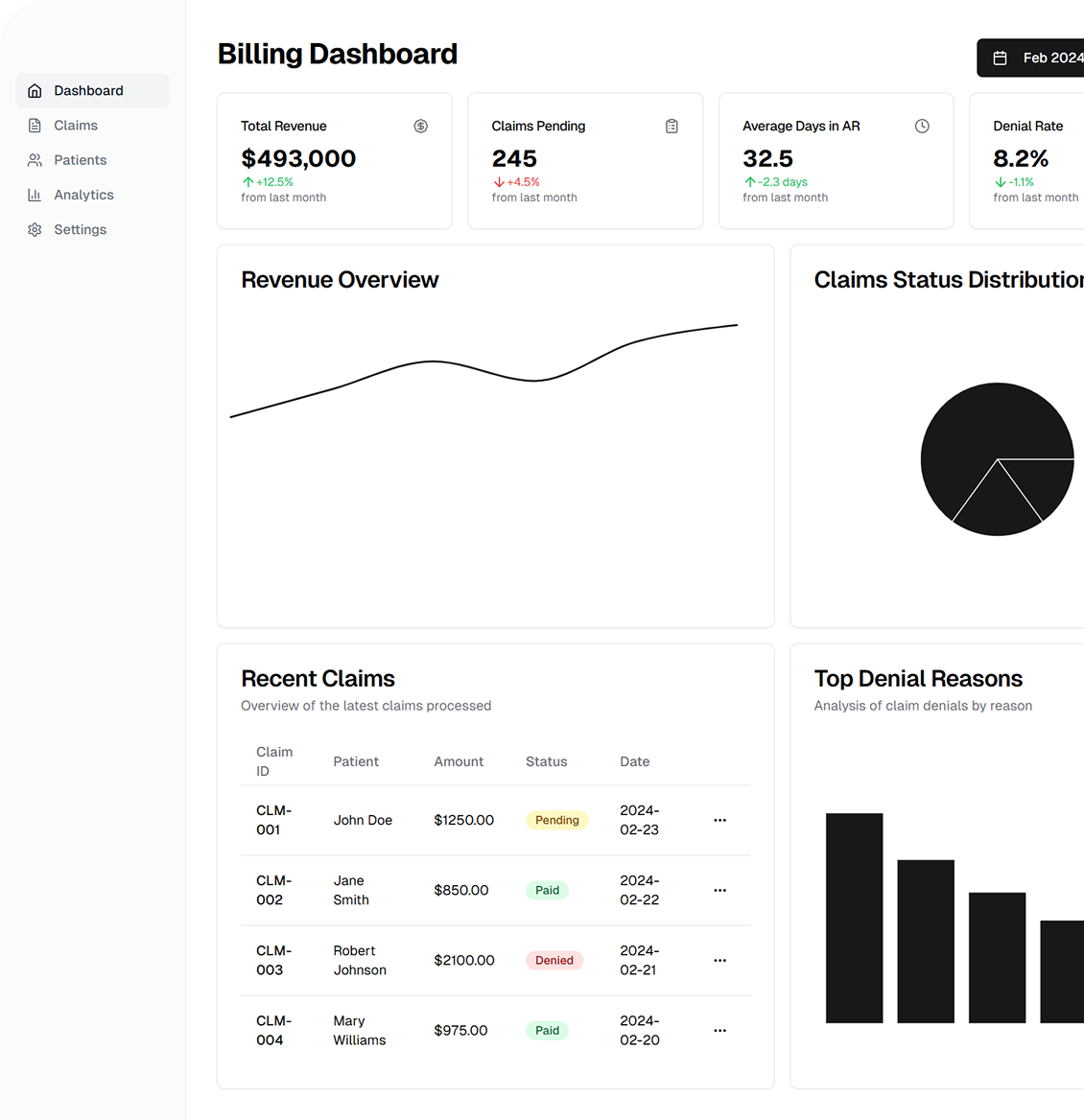
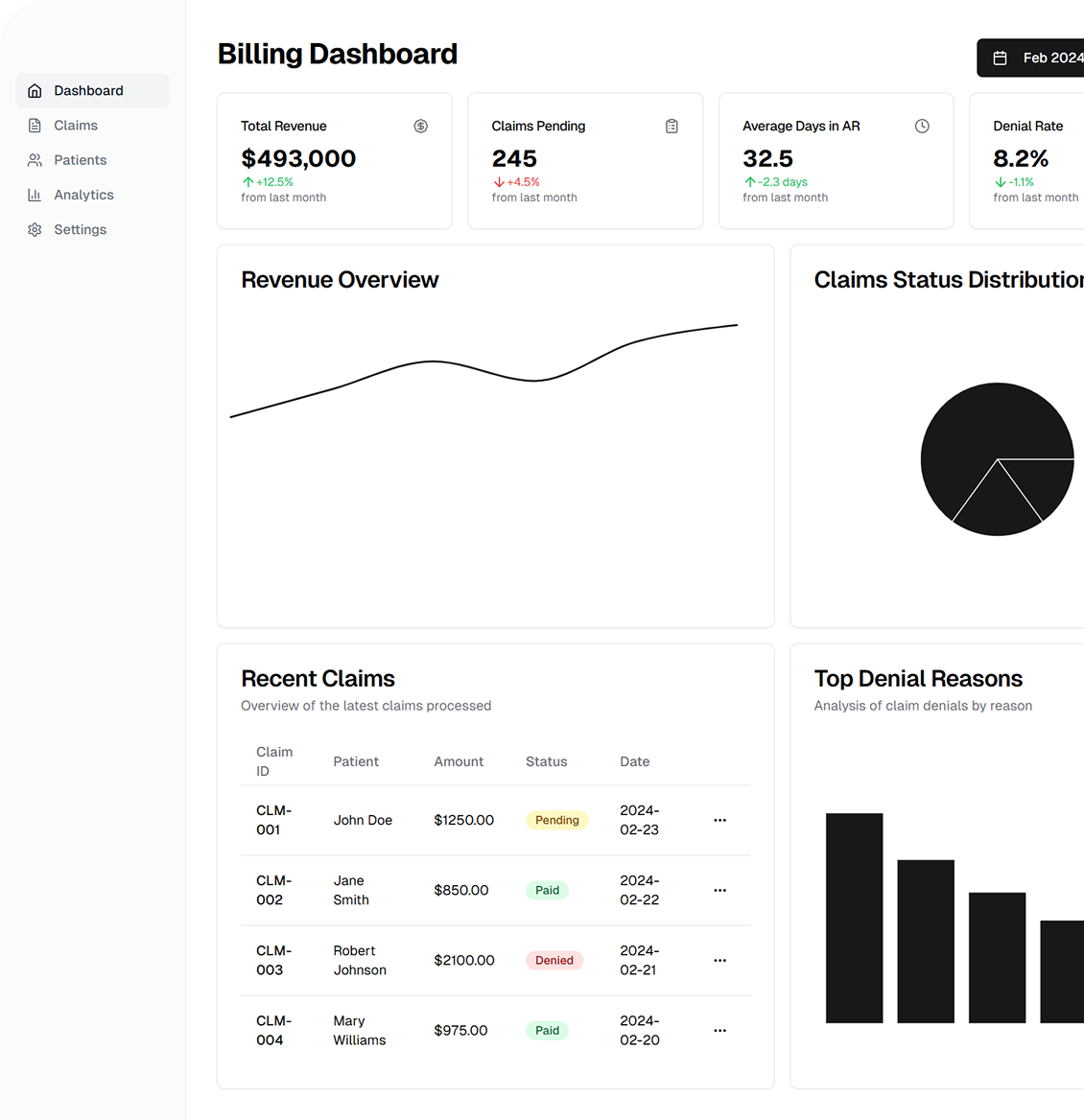
ASP‑RCM Solutions delivers comprehensive and up‑to‑date physician billing services, ensuring accurate data integration with your existing applications. Our services cover everything from billing and collections to No Surprise Act solutions—so you can focus on clinical duties while we handle the administrative details
Billing & Collections: End-to-end claims management. • No Surprise Act Solutions: Transparent cost estimates and fair billing. • Insurance AR Assortments: Prioritizing high-value claims. • Credit Balance Adjustments: Accurate refunds and balancing. • Payment Posting: Real-time EOB reconciliation. • Revenue Recovery: Follow-up on overdue accounts. • PMB Insurance Collections: Handling denied or partially paid claims.
Children’s Orthopedics & Emergency Care: OB‑GYN, heart disease, operations, etc. • General Practice Billing: Family practice, pediatrics, internal medicine. • Specialty Practice Billing: Oncology, neurology, dermatology. • Physician Groups Based in Hospitals: Emergency medicine, anesthesia, hospitalists, post‑acute care. • Our team is well‑versed in ICD, CPT, and HCPCS guidelines for each specialty.
Coding: AAPC-certified (ICD, CPT, HCPCS). • Claims: Daily filing. • Eligibility: Real-time verification. • Credentialing: Managed. • Rejections: Appeals handled. • Payouts: EOB review & deposits. • Balances: Invoice statements sent
We link seamlessly to your existing EHR or practice management system, employing real‑time data exchange (e.g., HL7 interfaces, secure APIs). This approach minimizes manual data entry, speeds up claim submission, and delivers robust billing analytics
HIPAA & Data Security: We ensure strict PHI protection. • No Surprise Act Compliance: Transparent cost-sharing to prevent surprise bills. • Audit Trails: Clear logs for accurate billing records. • Continuous Improvement: Regular audits to adapt to payer rule changes.
Our integrated RCM framework allows you to maintain a healthy bottom line. Each stage of operations—from eligibility checks to denial resolution—undergoes real‑time monitoring, ensuring consistent revenue flow and minimal administrative burdens
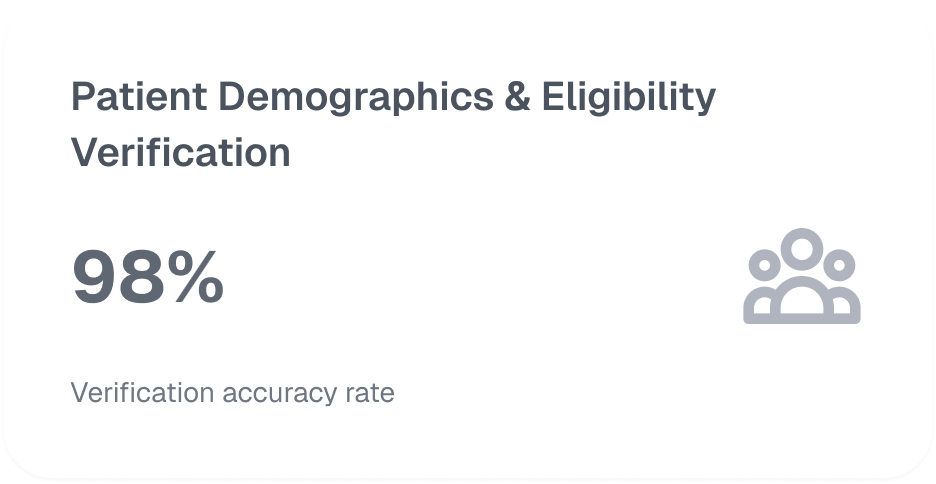
We capture and verify patient details in your EHR or billing system. This process includes real‑time checks for coverage limits, co‑pays, and prior authorization requirements to avert claim issues
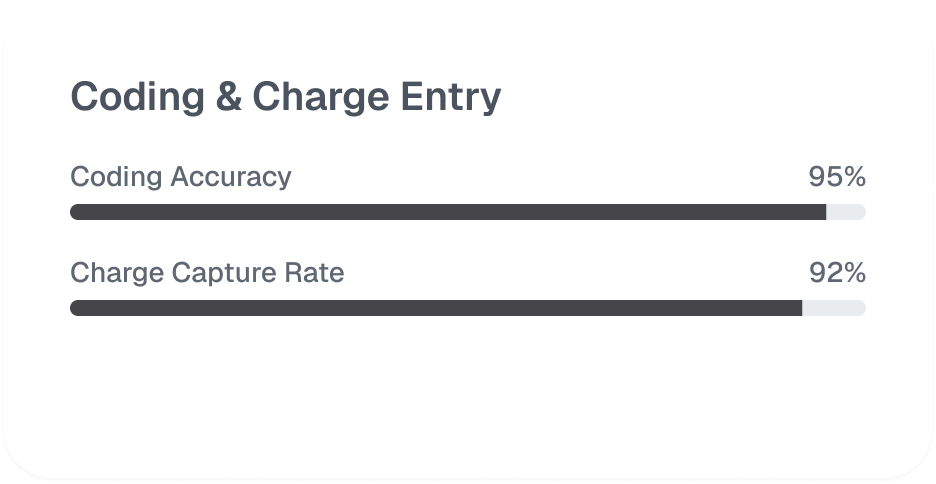
Our AAPC‑certified coders meticulously review provider documentation, assigning correct ICD, CPT, or HCPCS codes. Charges are then entered for swift submission, minimizing the chance of front‑end denials
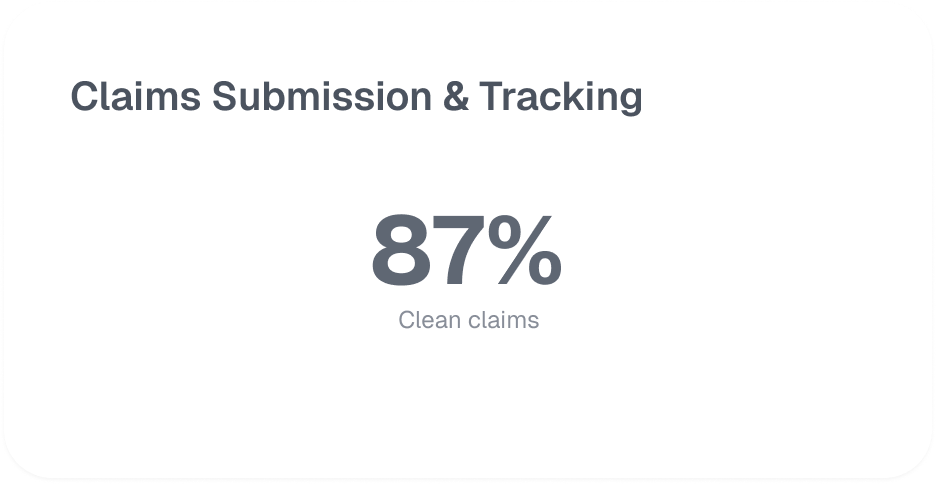
We electronically submit clean claims via 837P or 837I forms, depending on specialty. Automated trackers flag rejected claims for prompt resubmission, raising your first‑pass acceptance rate
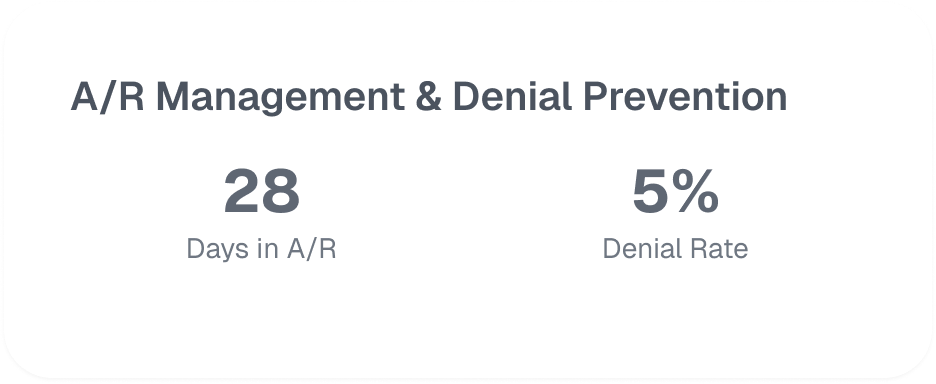
We categorize pending claims based on age and payer priority. Denial prevention teams identify trends—such as incorrect modifiers or missing documentation—and address them Proactively to reduce rejections
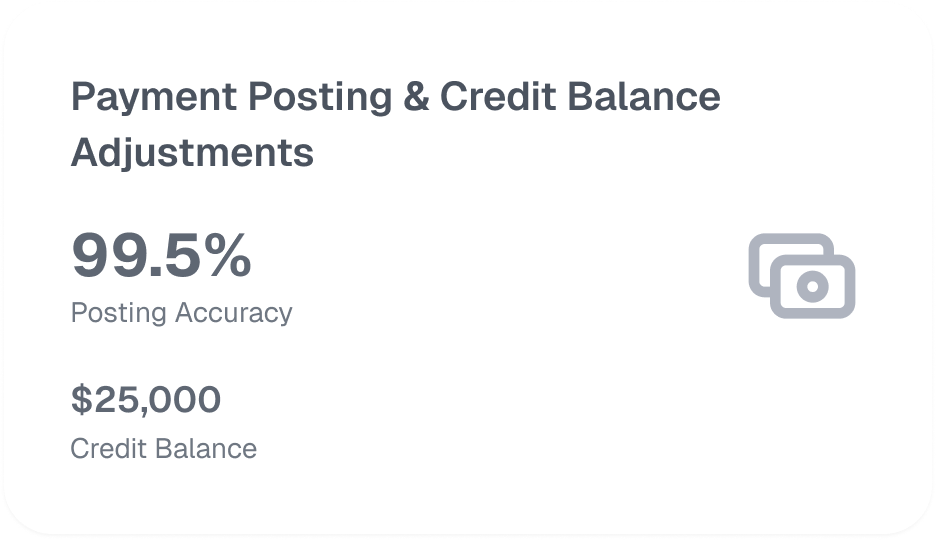
Received payments are matched against claims, capturing precise details of EOB statements. Overpayments or misallocations are swiftly corrected, ensuring accurate account balances and patient statements
We provide in‑depth analytics on clean claim rate, days in AR, and denial rates, alongside monthly compliance audits. This ensures ongoing revenue optimization and alignment with payers, regulators, and the No Surprise Act

.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers