BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
An extended business office experience that works seamlessly with your CBO leadership for breakthrough results
Schedule a CallTotal Charges Submitted
First-Pass Claim Acceptance Rate
Self-Pay Collection Rate
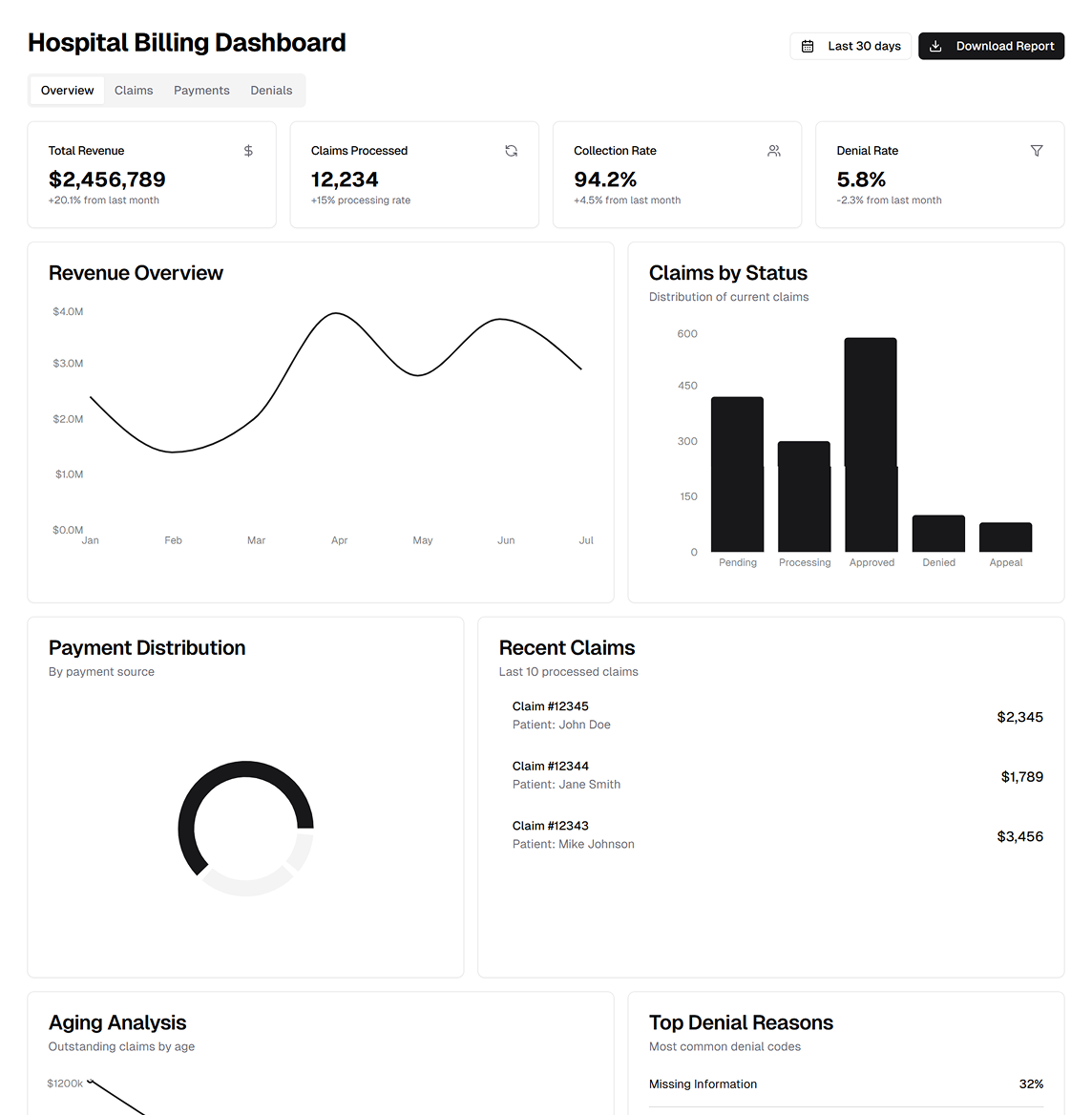
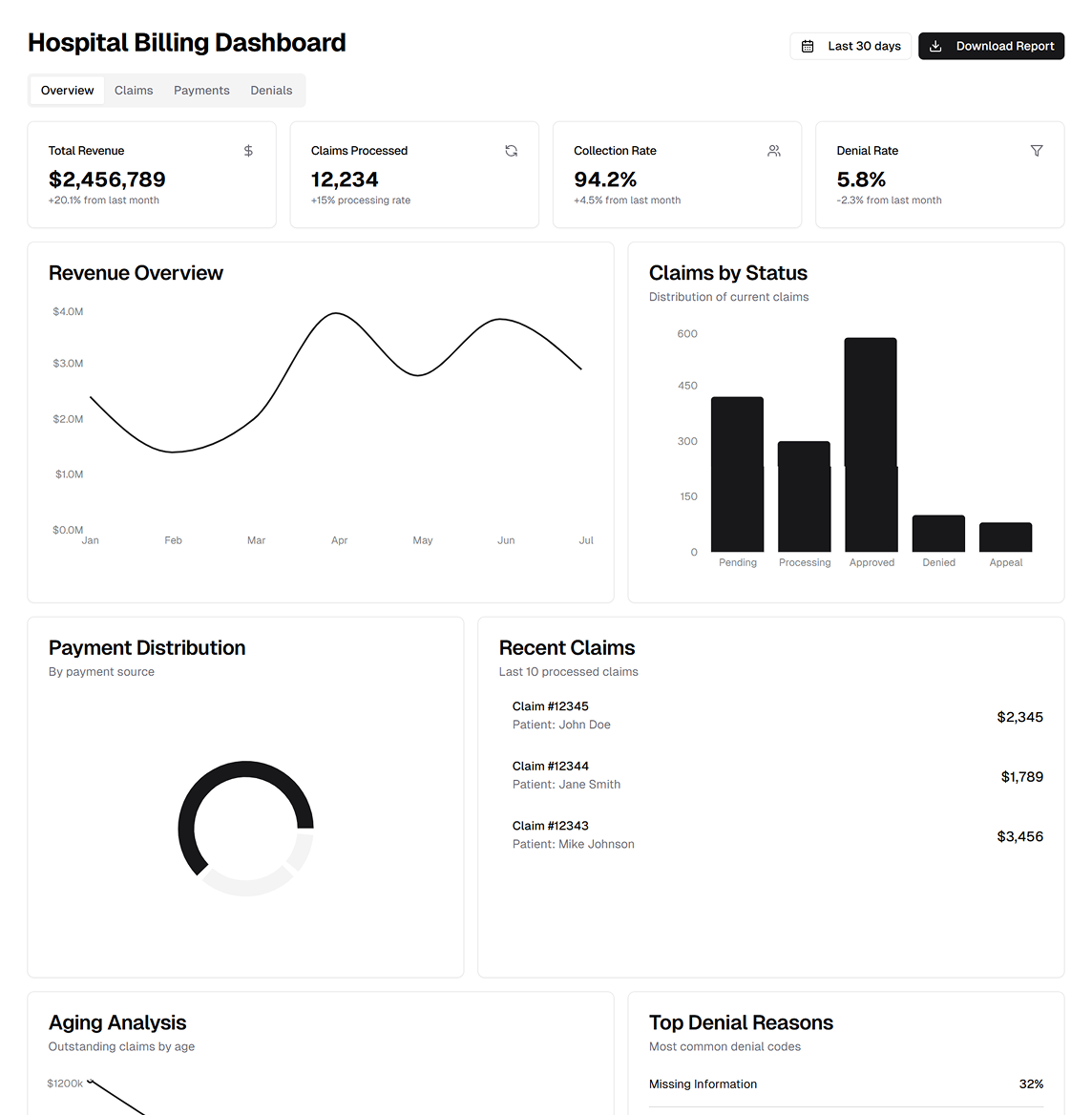
ASP-RCM Solutions helps hospitals streamline revenue cycle management, achieving measurable results based on HFMA KPI standards. Their team focuses on cost-effective, tech-driven hospital billing services, from insurance verification to accounts receivable follow-up
• Low Clean‑Claim Rate: High AR and denials disrupt cash flow, risking hospital operations. • Payer Delays: Slow reimbursements weaken revenue stability. • Complex Coding: Errors in CPT/ICD‑10 and DRG grouping lead to claim rejections. • Fragmented Systems: Poor integration hampers timely billing and collections.
• RCM Tracking & Trend Analysis: We identify patterns in denials and AR to pinpoint root causes, implementing real‑time fixes. • Dedicated Hospital RCM Staff: Skilled coders and billing specialists ensure accuracy, compliance, and an elevated first‑pass claim acceptance rate. • Proven Governance & Collaboration: Our structured approach fosters transparency between your hospital leadership and our extended business office services
• Patient Insurance Verification • Patient Demographic Entry • CPT/ICD‑10 Coding • Charge Entry • Claim Submission • Payment Posting • Account Receivable Follow‑Up • Denial Management • Reporting & Analytics
• Insurance Verification • Medical Coding • Charge Entry • Payment Posting • Rejection Management • AR Follow-Up • Credit Balances
• Lower Collection Costs • 98% First‑Pass Acceptance • Boost Net Collections • Value‑Based Care Support • High-Impact Cash Flow • Quality Medical Billing • HFMA KPI Tracking
Our hospital billing operations leverage modern EHR integrations, HL7 interfaces, and robust data‑driven analytics to minimize denials, shrink AR, and improve overall revenue cycle outcomes—while staying firmly within HIPAA and data security guidelines
We employ certified CPT/ICD‑10 coders to accurately convert clinical documentation into billable charges. Using advanced coding validation tools and DRG logic, we reduce the risk of rejections, leading to faster reimbursements
Our denial prevention teams continuously analyze payer trends, identify coding or documentation gaps, and deploy immediate solutions. Automated trackers alert staff to pending AR accounts, enabling swift appeals and underpayment recoupment
Customizable dashboards measure performance across key HFMA KPI metrics such as clean claim rate, days in AR, and net collection rate. This real‑time visibility keeps your leadership fully informed of ongoing improvements
We follow strict data encryption, ** SOC 2** best practices, and periodic security audits to protect sensitive PHI. By adhering to HIPAA standards, we ensure safe transmissions of EDI files and claim attachments
We seamlessly interface with various EHRs and practice management systems via HL7 or API connections, unifying front‑end patient data with back‑end billing workflows for a frictionless RCM experience
Our partnership model positions us as an extended business office for your hospital. Lean methodologies, ongoing staff training, and process optimization keep your billing cycle efficient and adaptable to ever‑changing payer requirements
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers