BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Boost Cash Flow and Streamline ED Revenue Cycle Management
Schedule a CallCritical Care Reimbursement Rate
Average Time to Submit ER Claims
Denial Rate for Level 4 & 5 ER Visits
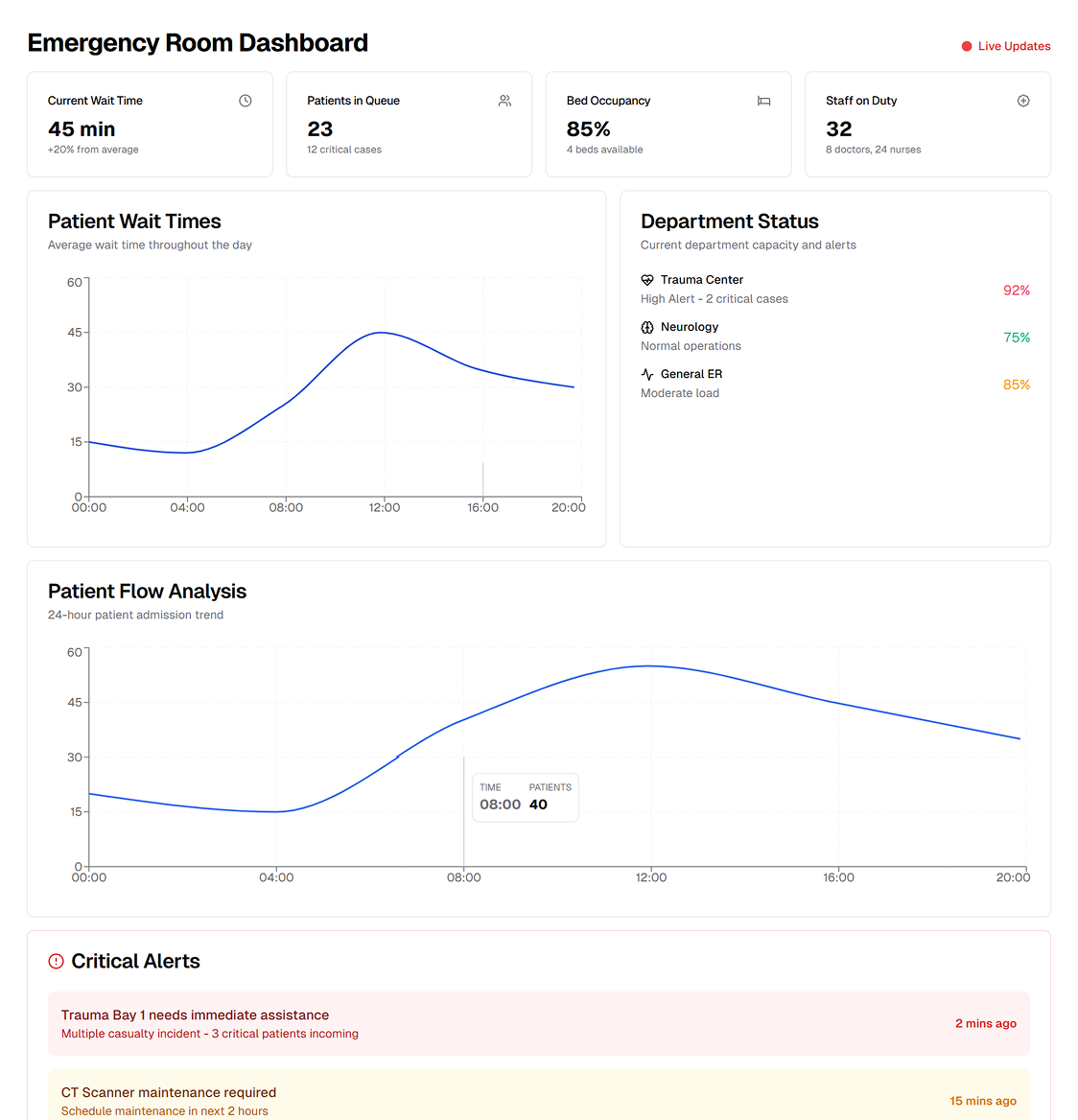
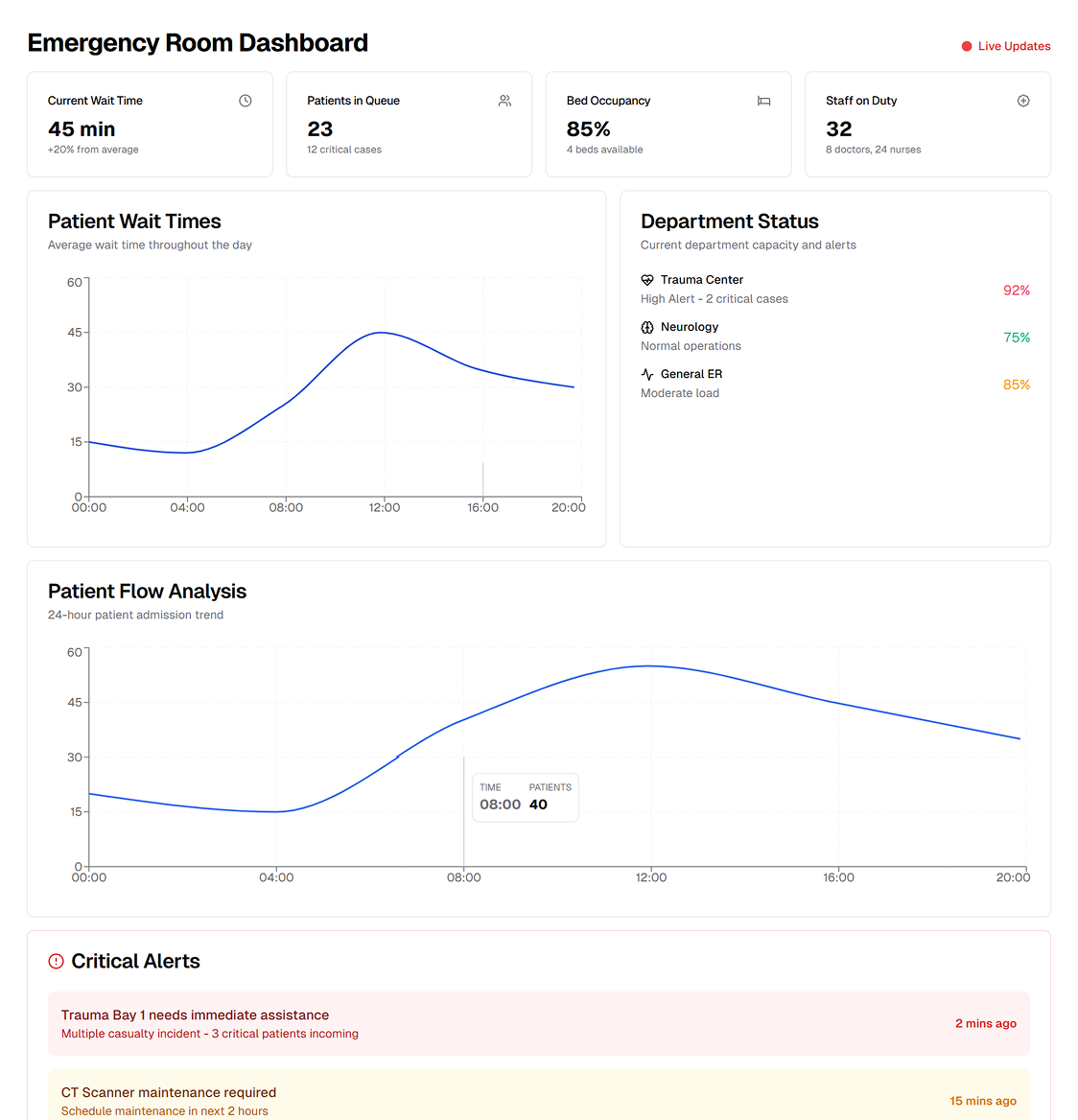
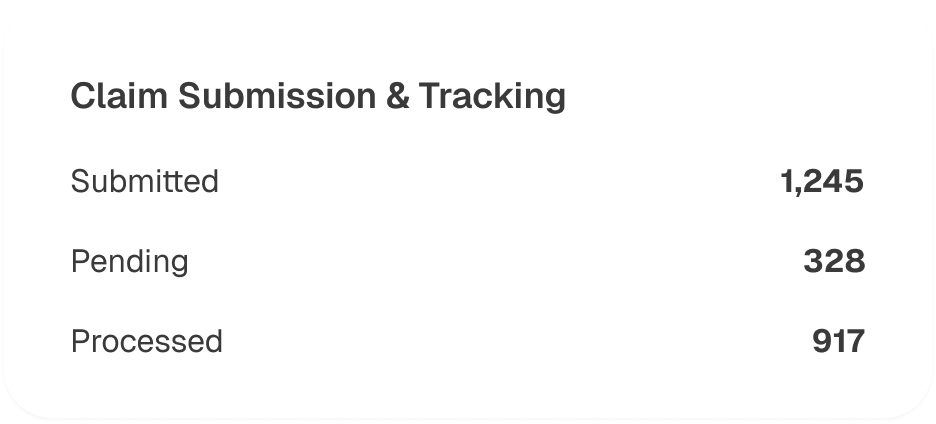
Recent healthcare reforms and shifting CMS guidelines have put tremendous pressure on group practices in emergency departments to deliver high‐quality care while maintaining stable cash flow. Complex CPT and ICD‐10 coding requirements, combined with compliance obligations such as HIPAA and EMTALA, can make in‐house billing unpredictable and time‐consuming. Our integrated billing solution alleviates these burdens by standardizing coding procedures, implementing robust denial management tactics, and leveraging advanced analytics to elevate your bottom line.
Emergency departments often lose revenue through insufficient documentation, inadequate credentialing, and coding inaccuracies—particularly for unspecified diagnoses. We tackle these pitfalls by improving reporting documentation, training your staff on procedure code best practices, and ensuring each claim is coded to reflect the correct level of service. This diligent approach helps reduce underpayments and avoid recurrent denials
Clear, detailed documentation is key to accurate billing for emergency care services. Our team works closely with your ED staff to implement robust quality assurance procedures, ensuring that every patient encounter is properly recorded. By refining physician documentation and mapping them to the most relevant CPT and ICD‐10 codes, we minimize claim rejections and maximize reimbursements
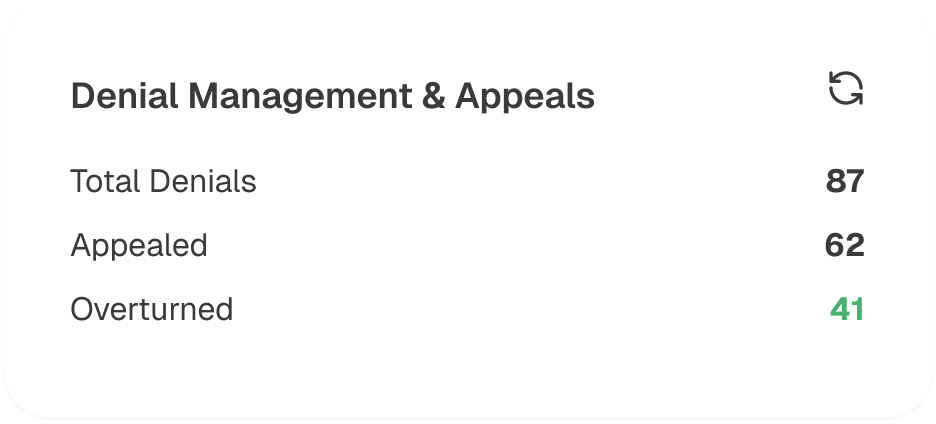
Our proactive denial management strategy includes roo’’ jbb, cause analysis, rapid reprocessing of underpaid claims, drafting appeals per AMA and CMS guidelines, and ongoing staff education on diagnoses and coding
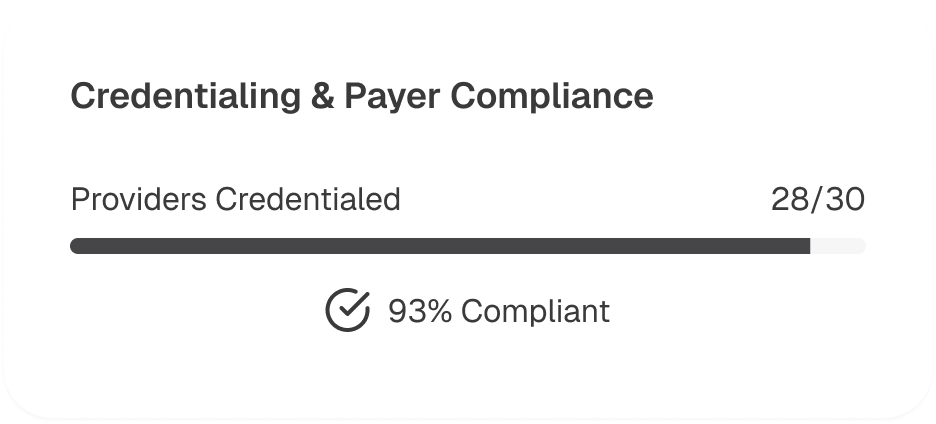
Emergency departments typically serve a wide payer mix. Ensuring that every clinician is properly credentialed with your region’s dominant insurers is essential for timely and full reimbursement. We manage the payer credentialing process—from initial applications to periodic revalidations—reducing administrative hurdles and cutting down on claim delays caused by incomplete or expired enrollments
We collaborate with your ED to establish stringent QA procedures and investigate issues such as false allegations or billing discrepancies. By maintaining compliance with HIPAA, EMTALA, and other regulatory requirements, we protect both your patients and your practice. In turn, this proactive stance not only curbs legal exposure but also preserves your revenue integrity
Our proven operational model addresses the full scope of Emergency Department RCM, from charge capture to payment posting. By combining specialized ED coding expertise, advanced billing technology, and continual staff education, we create a more resilient and profitable revenue cycle for group practices
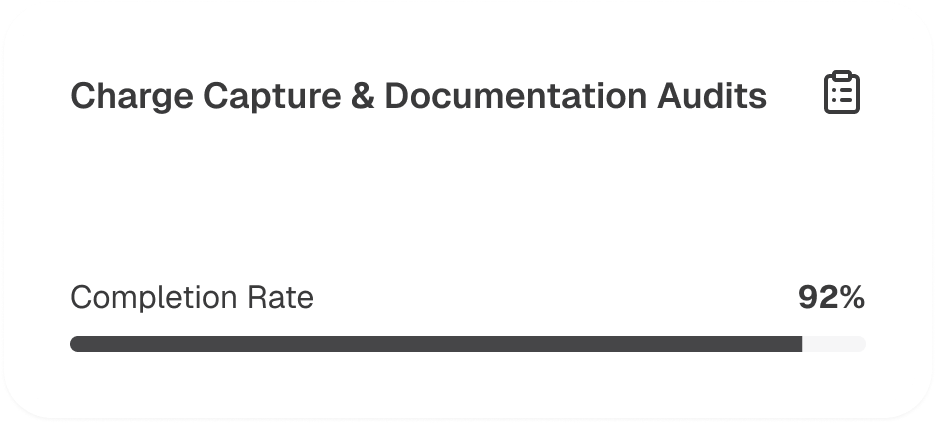
We ensure each patient encounter—whether a level‐2 or level‐5 ED visit—is captured promptly with the correct E/M codes. Periodic documentation audits verify that your clinicians meet the standards of medical necessity and completeness required by payers and CMS guidelines
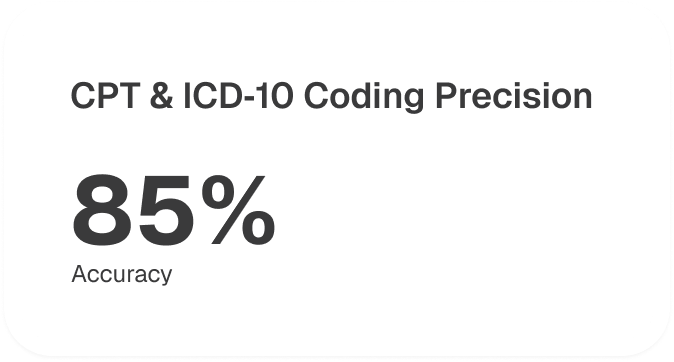
Our certified coders translate clinical notes into the most up‐to‐date CPT and ICD‐10 codes, applying any necessary modifiers. This meticulous coding process prevents “unspecified” labels, which are frequent triggers for claim rejections or down‐coding by payers
We utilize cutting‐edge billing software to transmit claims electronically and monitor their status in real time. Automation identifies potential errors before submission—like missing referral numbers or incorrect place of service codes—reducing the likelihood of rejections and rework
When denials occur, our specialists immediately perform a root‐cause analysis to resolve coding, documentation, or credentialing issues. We then file appeals backed by robust documentation, focusing on underpayment recovery and secondary claim resolution to maintain a steady cash flow
We manage payer enrollment for all your ED providers, staying on top of renewals and changes in payer policies. This ensures that every physician is recognized by major insurers—streamlining pre‐claim checks and reducing hold‐ups caused by incomplete credentialing
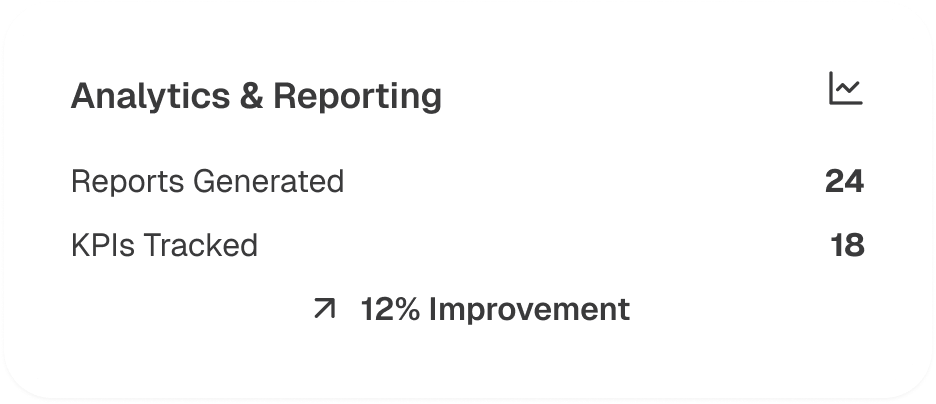
Our analytics dashboards deliver insight into key performance metrics, such as claim acceptance rates, days in AR, and average reimbursement per visit. Regular reporting uncovers trends and areas for improvement, enabling us to refine training, documentation, or coding workflows to continually enhance your ED’s financial performance
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers