BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Primary-Care Revenue, Handled by Primary-Care Specialists
Schedule a CallTotal Payer & Patient Collections
Avg Time for E/M Code Claim Processing
Denial Rate
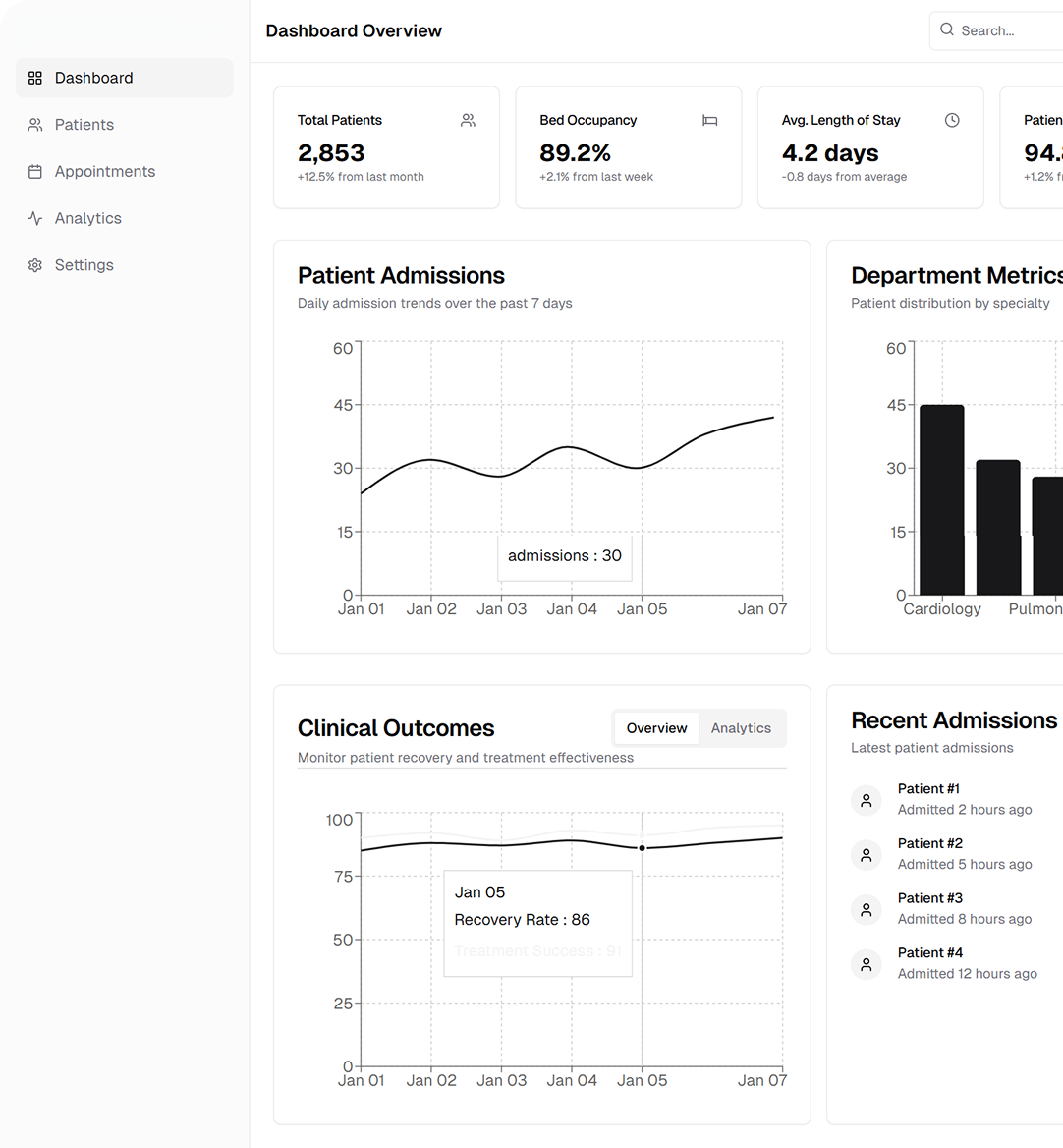
Manual chart reviews align visit levels with regularly AMA guidelines, eliminating down-coding and audit exposure.
From complex, multi-problem E/M visits to chronic-care add-ons, we capture every legitimate dollar while guarding against payer audits.
Accurate CCM, TCM, AWV, and Principal Care Management coding boosts revenue without burdening clinicians.
Line-item reviews ensure persistent conditions are documented and coded each year, driving fair RAF scores.
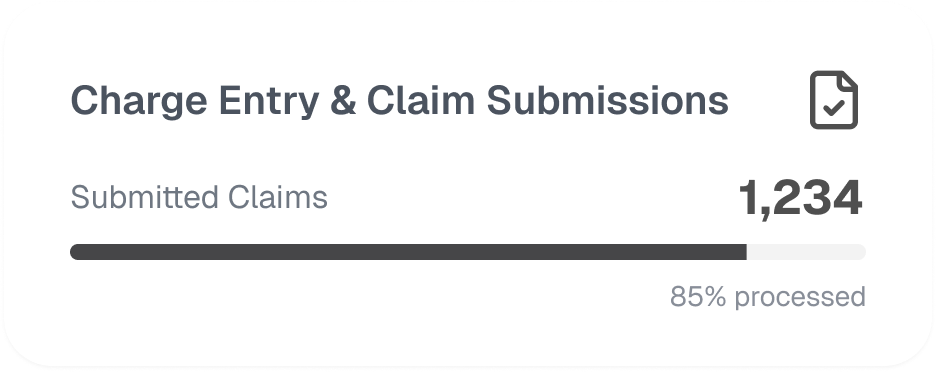
Root-cause analysis, same-day refiling, and seasoned phone appeals cut the denial rate and shrink days-in-AR.
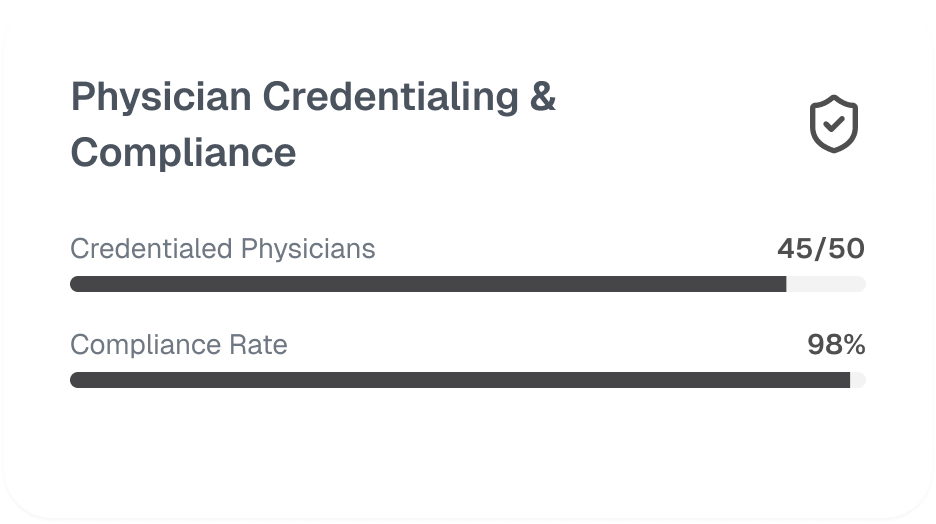
Quarterly coding audits and 1:1 physician feedback keep the team current on CMS, MAC, and LCD policy shifts.
Our AAPC-certified coders, former practice managers, and denial specialists breathe internal medicine.
We lock in contracts, update CAQH, and negotiate fee bumps.
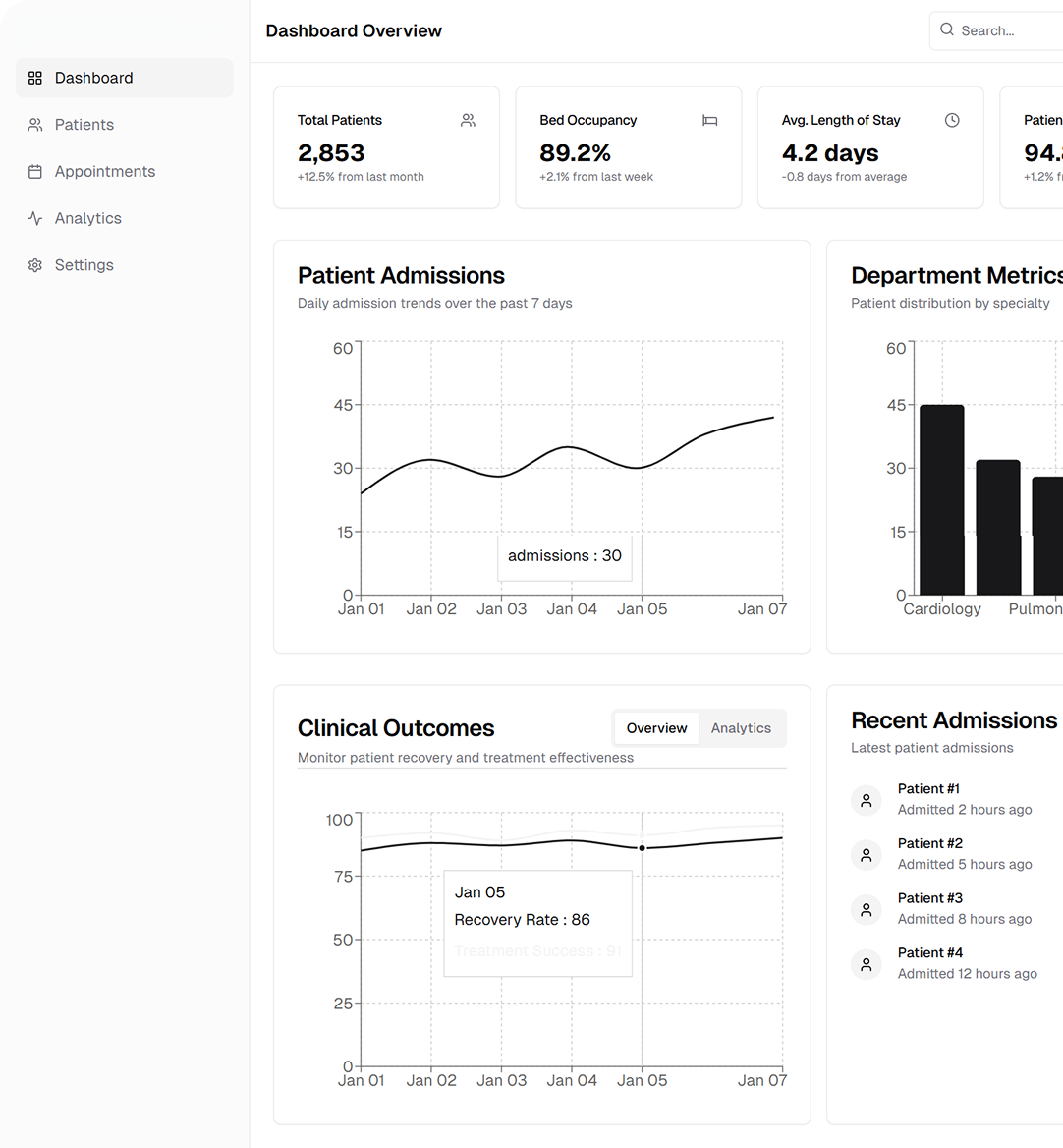
Certified coders match ICD-10 + CPT + HCPCS to each encounter—no “EHR autopilot.”
Manual scrubs catch modifier misfires, NCCI edits, and CCI bundling issues before files hit the clearinghouse.
Dedicated reps call payers, cite policy, and push appeals until the check clears.
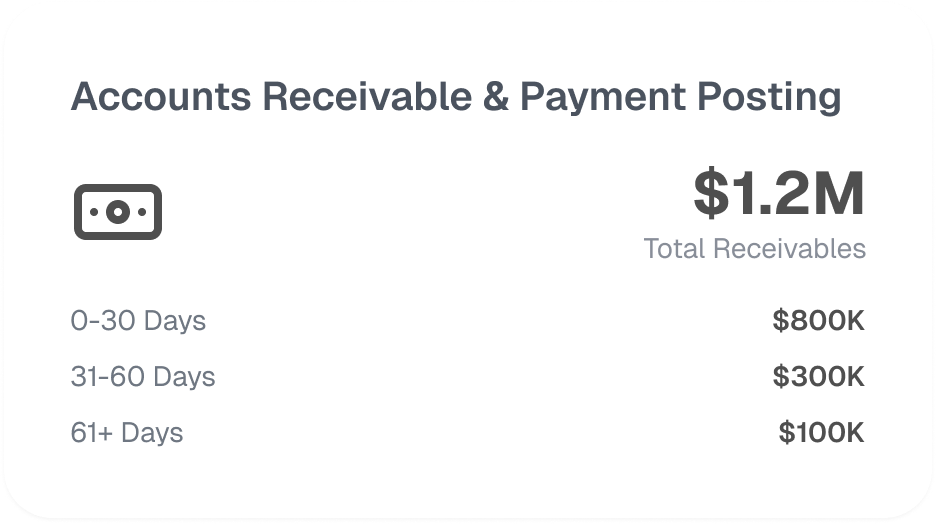
Executive KPI packet, action plan to review net collection %, denial reasons, payer lag—and map next-step fixes.
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers