BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Engage with a provider that offers back‑office expertise to enhance your financial outcomes and streamline coding operations
Schedule a CallTotal Charts Coded
Coding Accuracy Rate
Coding-Related Denial Rate
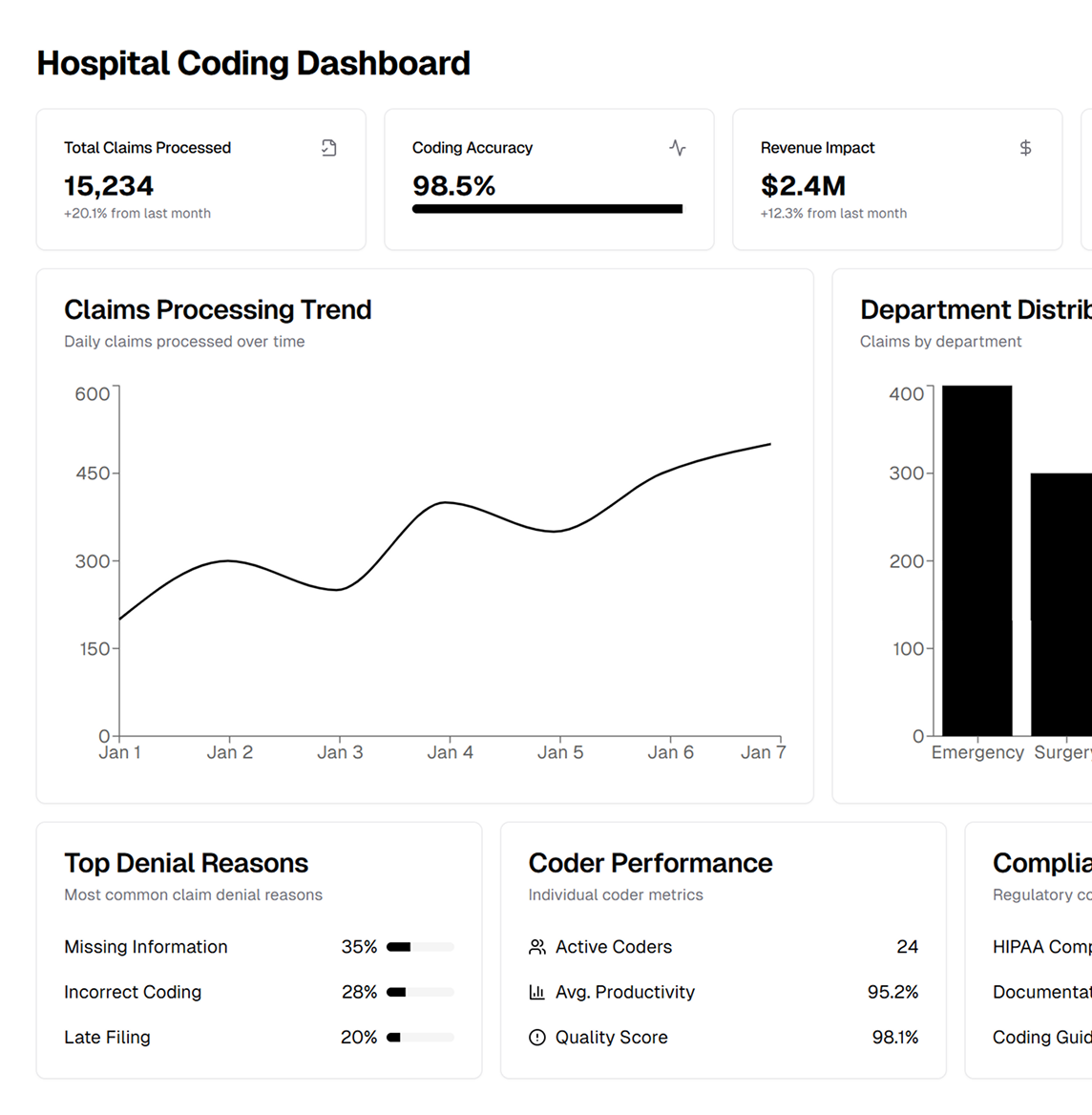
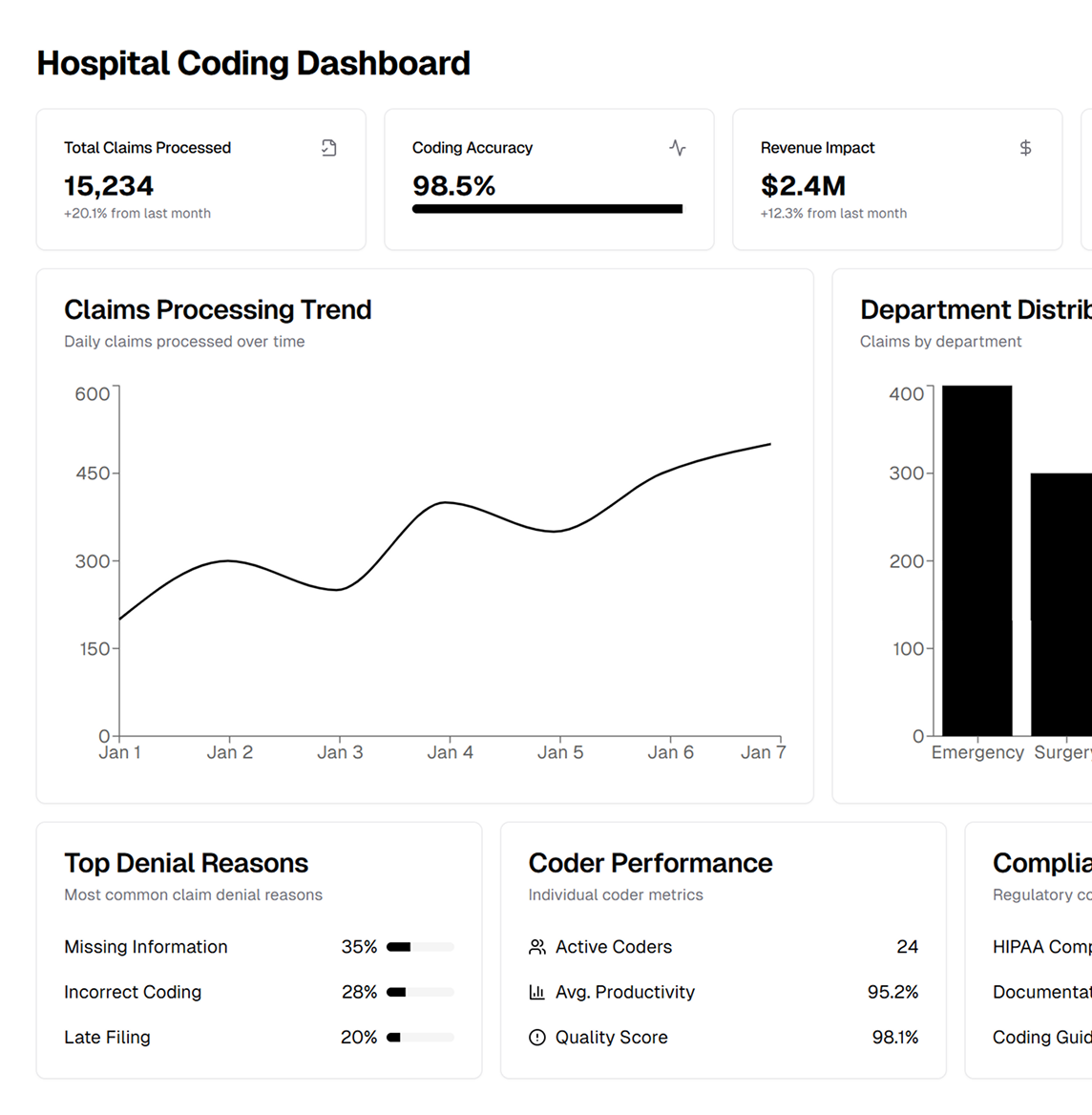
ASP-RCM Solutions offers top-tier remote medical coding services, using certified coders to ensure compliance, minimize denials, and expedite reimbursement. They integrate technology and professional expertise for seamless integration into HIM department workflows
Our coding solutions are tailored to specific facilities, including: • Academic Medical Centers • Critical Access Hospitals • PPS Hospitals • Ambulatory Surgery Centers • Independent Emergency Departments We ensure that all coding aligns with facility-specific procedures, payer regulations, and compliance requirements.
We offer a full suite of coding services to support every aspect of your hospital’s revenue cycle management (RCM): • Certified ICD‑10 coders and trained trainers. • Corporate Coding Quality Programs to ensure compliance. • Direct communication with project managers for operational clarity. • Secure coding with access to IT systems or secure ASP environments. • Flexible staffing for weekends, holidays, or urgent needs. • Real-time DNFB/DNFC reporting to reduce backlogs.
Partnering with ASP‑RCM delivers quantifiable improvements: • Lower DNFB/DNFC rates with streamlined billing • Higher CMI for better DRG reimbursements • Optimized cash flow via real-time coding audits • Reduced risks from payer rules and coder shortages.
Our approach focuses on precision and accountability to: • Enhance coding accuracy for better reimbursement. • Minimize compliance risks and audit exposure. • Identify coding gaps to reduce denied claims. • Boost productivity through continuous audits.
Leverage our technology stack for seamless coding and reporting: • AI-powered claim checks and coding validation • EHR integration for real-time updates • HIPAA-compliant encryption • Analytics dashboards for KPIs
Our end-to-end coding operations are built on a foundation of cutting-edge tools, skilled coders, and strict compliance with regulatory mandates. From pre-submission audits to denial resolution, we handle every step with precision and transparency
We tailor HIM coding services to meet the specific needs of your facility, ensuring accurate documentation, seamless payer submissions, and minimized coding rejections
Our secure IT platforms allow remote coders to work within your system safely, maintaining data privacy and preventing unauthorized access, in compliance with HIPAA
We track outstanding claims, focusing on discharged-not-final-billed (DNFB) accounts to reduce backlog and maintain healthy cash flow for your facility
By analyzing denial trends, our experts quickly address the root causes of rejected claims, such as incorrect codes or incomplete documentation, to maximize reimbursements
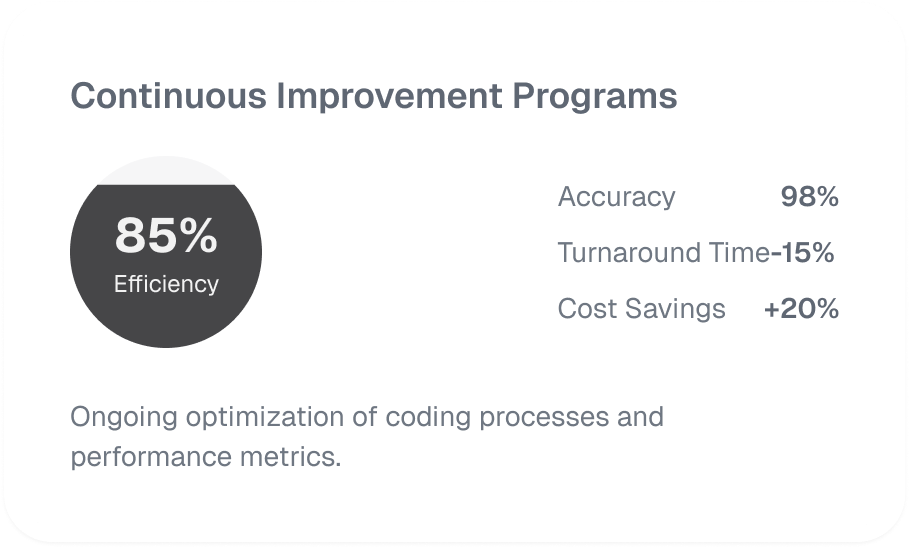
Our team conducts ongoing coding audits and performance assessments, ensuring your operations remain adaptable to ICD‑10 changes, payer rule updates, and compliance mandates
We seamlessly integrate coding workflows with your EHR systems via HL7 interfaces or APIs, streamlining front- and back-office processes for enhanced efficiency
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers