BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Achieve Financial Stability and Operational Excellence in a Post-COVID Urgent Care Landscape
Schedule a CallDOS to Claim Release
In A/R
POS Collection Rate
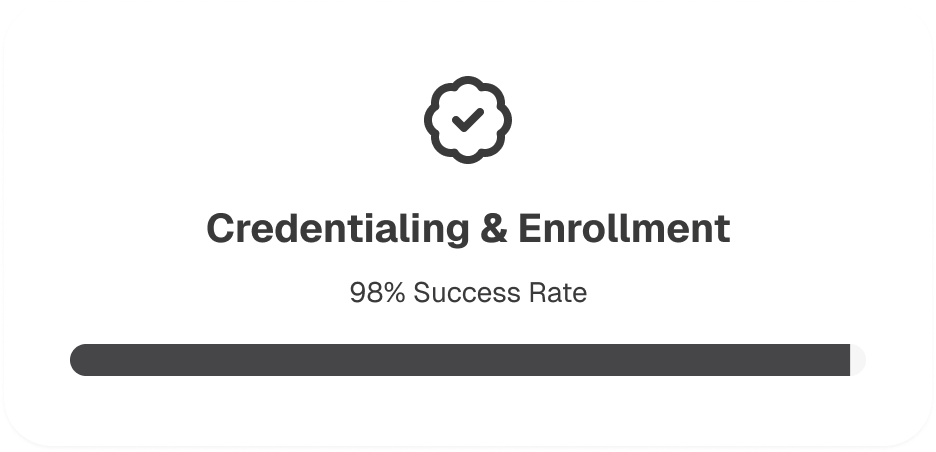
ASP-RCM Solutions addresses post-COVID challenges in urgent care centers by implementing customized strategies for financial stability and operational efficiency, including streamlined credentialing and advanced patient flow management
ASP-RCM uses digital workflows and specialized expertise to expedite provider enrollment, reduce wait times, and establish a steady revenue stream for urgent care centers
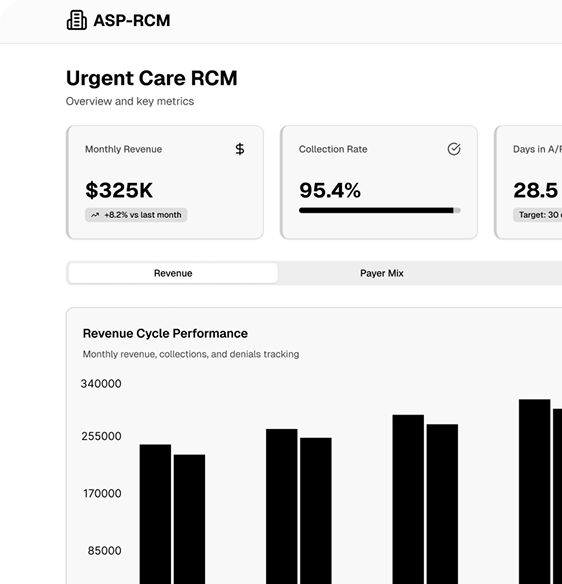
ASP-RCM optimizes patient flow, reduces wait times, and maintains patient satisfaction by utilizing real-time eligibility verification and prior authorization tools in centers with evolving patient behaviors
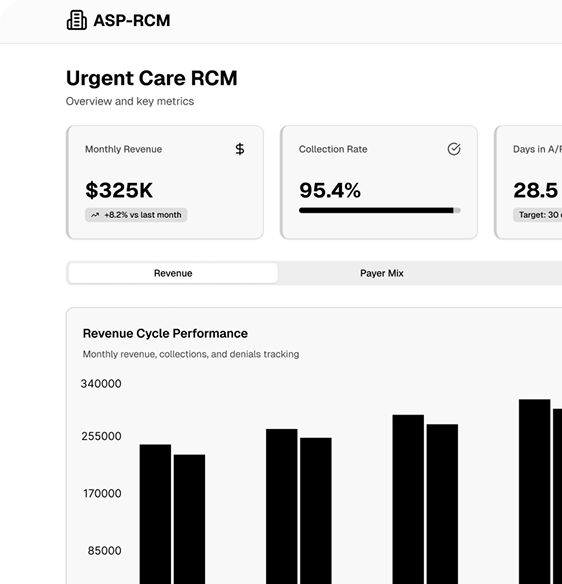
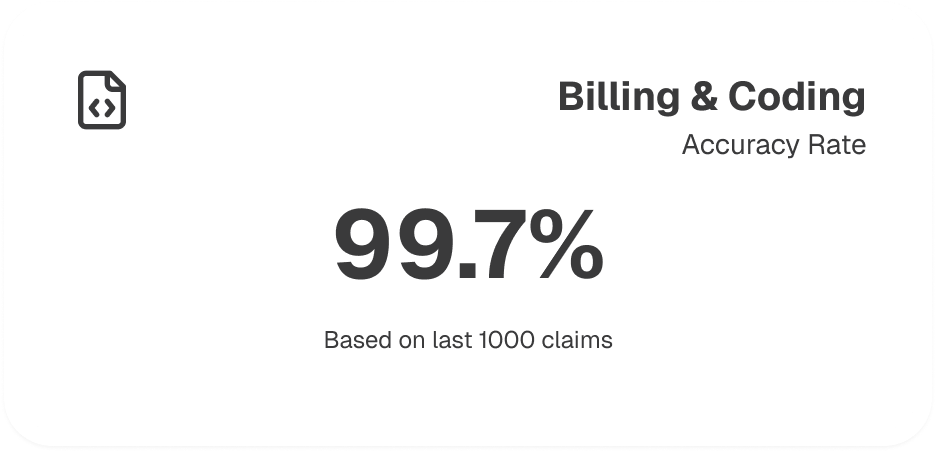
ASP-RCM's revenue cycle management suite, including billing, coding, claims submission automation, and data analytics, caters to urgent care needs, allowing providers to focus on patient care
Our approach utilizes advanced RCM software, streamlined workflows, EHR integration, HL7 data exchange, and KPI dashboards to optimize revenue cycles, enhance patient satisfaction, and scale with urgent care growth
Our simplified revenue loss process helps identify credentialing issues, enhances payer negotiation skills, and supports the expansion of urgent care networks with flexible solutions.
ASP-RCM’s end-to-end operational framework covers every aspect of urgent care revenue cycle management—from pre-visit eligibility checks to final payment reconciliation—using robust automation, compliance-focused processes, and data-driven insights
We expedite provider onboarding by proactively managing CAQH profiles, monitoring NPPES listings, and collaborating with payers for quick network inclusion. This reduces revenue delays and ensures new or expanding urgent care practices can serve patients without unnecessary holdups
Our certified coders use specialty-specific CPT, ICD-10, and HCPCS guidelines to minimize coding errors, while automated scrubbers catch discrepancies before claim submission. This precision leads to fewer claim denials and faster reimbursements
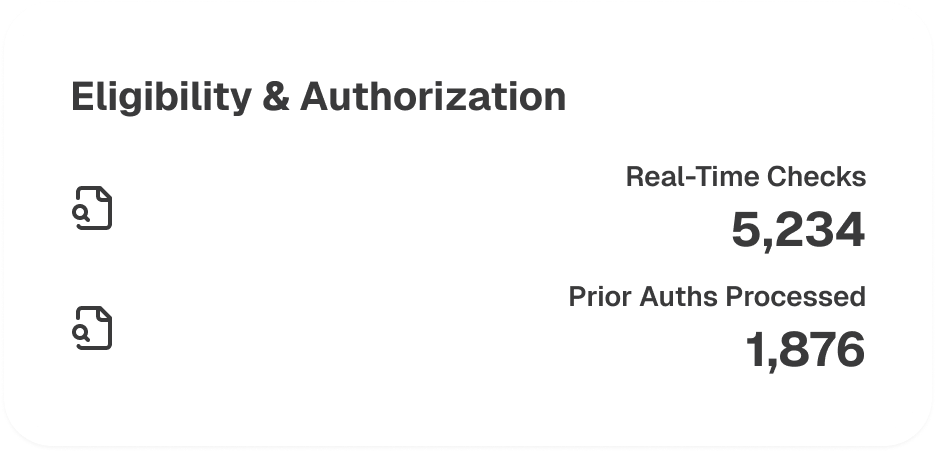
By integrating API-based tools and payer portals, we confirm patient coverage and secure prior authorizations in real time. This proactive approach prevents coverage surprises, reduces wait times, and ensures seamless patient experiences
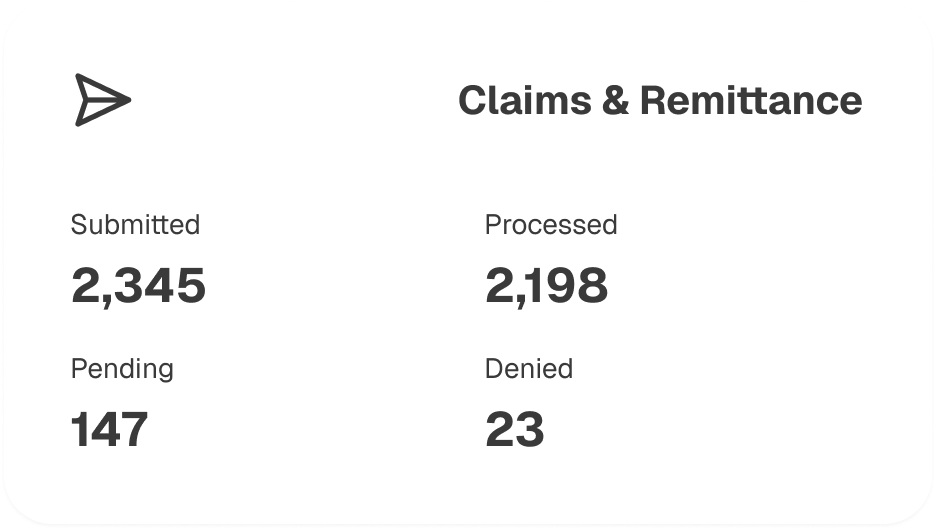
We handle electronic claims submission through secure clearinghouses, track remittance advice (ERA), and reconcile payments to ensure full reimbursement. Automated processes and electronic fund transfer (EFT) setups expedite revenue flow, while robust payment posting ensures accurate accounting
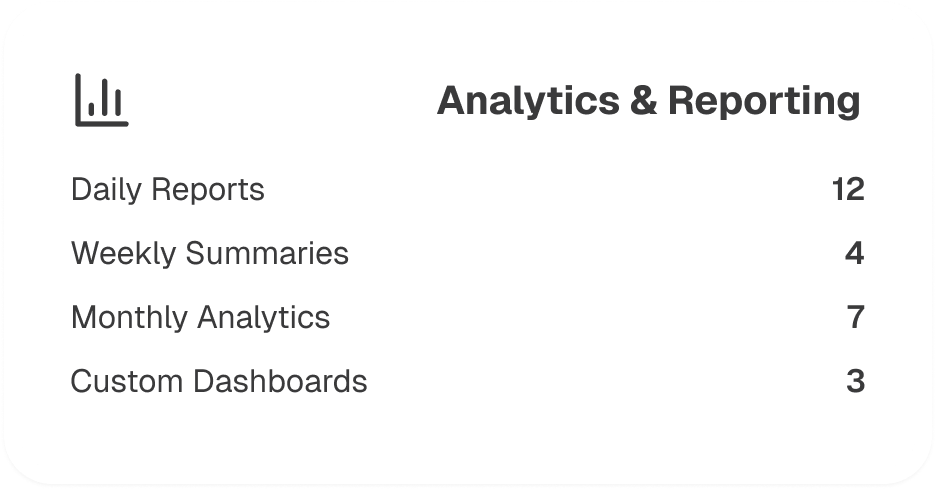
ASP-RCM deploys KPI dashboards and customizable reports that provide insights into claim status, reimbursement trends, and revenue forecasts. These analytics help urgent care centers identify improvement areas, detect potential fraud, and make data-driven decisions to enhance profitability
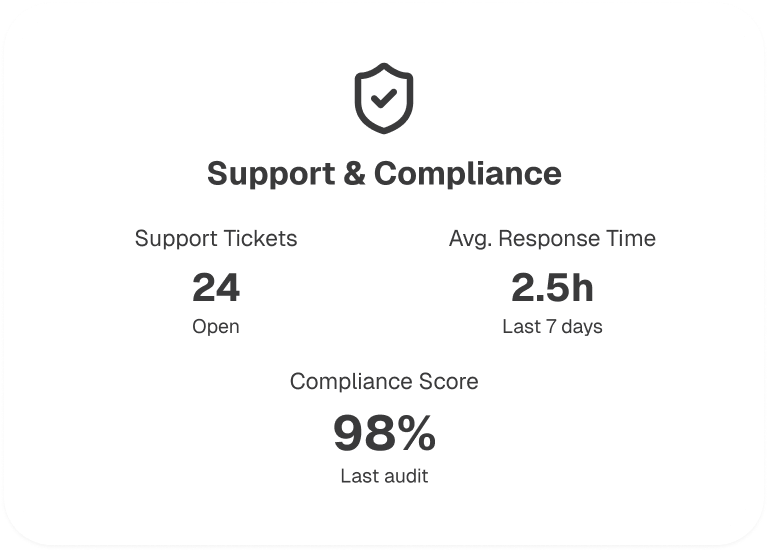
We maintain strict HIPAA compliance throughout all RCM processes and offer continuous support for credentialing updates, re-credentialing, and contract renegotiations. Regular audits and compliance checks help your practice stay aligned with evolving regulations and payer requirements
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers