BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Navigating Insurance with Obstetric and Gynecologic Finesse
Schedule a CallTotal Maternity & GYN Visits Billed
Prenatal & Delivery Claim Approval Rate
Insurance Coverage Issues for Infertility Treatments
OB/GYN practices face billing and coding complexities due to services like family planning, anesthesia, and abortion tests. Our AAPC-certified coders ensure compliance with CMS, AMA, and insurance requirements, resulting in faster reimbursement cycles and accurate claims submissions
Depending on your clinic’s insurance mix, our dedicated OB/GYN billers optimize claim cycles to 21–25 days and immediately follow up on unpaid claims older than 18 days. We handle both print and electronic submissions, ensuring that no claim falls through the cracks. Our vigilant approach to pre‐authorization and denial management accelerates cash flow and keeps your practice financially healthy
From CPT codes used in deliveries, surgeries, and anesthesia management to ICD‐10 diagnostic specificity for gynecologic conditions, accurate coding is the bedrock of timely reimbursements. Our team’s in‐depth knowledge of HCPCS rules, as well as advanced E&M coding strategies, ensures every service—from mother‐fetal medicine to reproductive endocrinology—is billed correctly the first time
With 10+ years of experience supporting OB-GYN practices, our expert coders specialize in: • Mother-Fetal Medicine • Fertility & Reproductive Endocrinology • Pelvic Reconstructive & Uro-Gynecology • Laparoscopic Procedures • Family Planning • Pediatric & Adolescent Gynecology • Geriatric & Menopausal Gynecology
Staying updated with CMS policies, AMA guidelines, and shifting payer requirements is essential for OB/GYN providers. Our rigorous compliance measures, including HIPAA safeguards, ensure patient data protection and smoother claim acceptance. By automating claims tracking and error checks, we maintain a 98% first pass claim approval rate, significantly reducing rework and delays
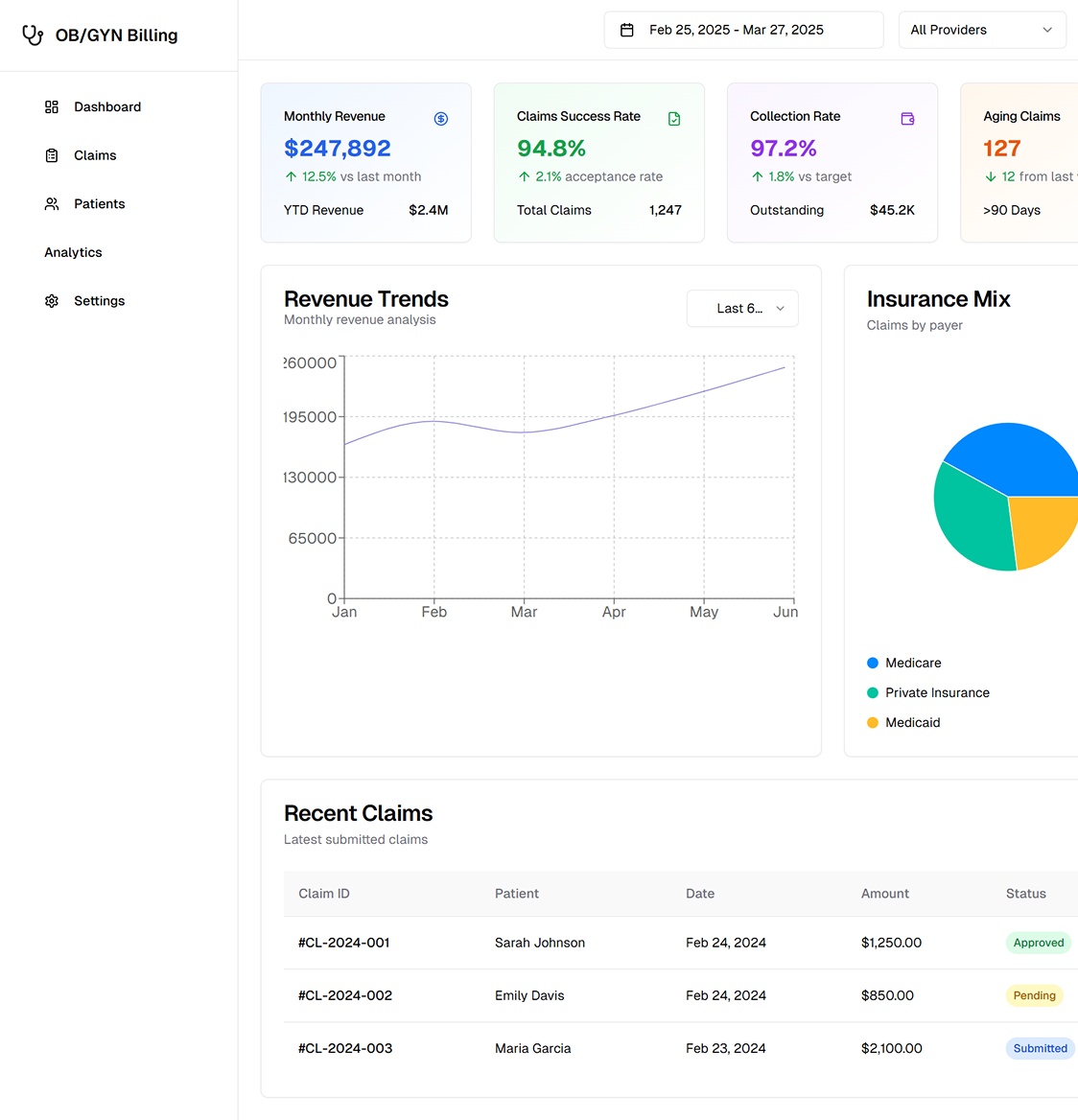
Our specialized approach to OB/GYN billing delivers tangible results: • Increase in net revenue through precise coding and timely follow‐ups • Improved 24/7 workflow and real‐time dashboards for regulatory compliance • Dedicated teams skilled at OB/GYN billing strategies, ensuring claim accuracy • Uniform RCM procedures that integrate seamlessly with your existing systems
We combine state‐of‐the‐art billing software, specialized OB/GYN coding expertise, and consistent follow‐ups to help you optimize reimbursements. Each step—from charge entry to payment posting—is standardized for accuracy and speed
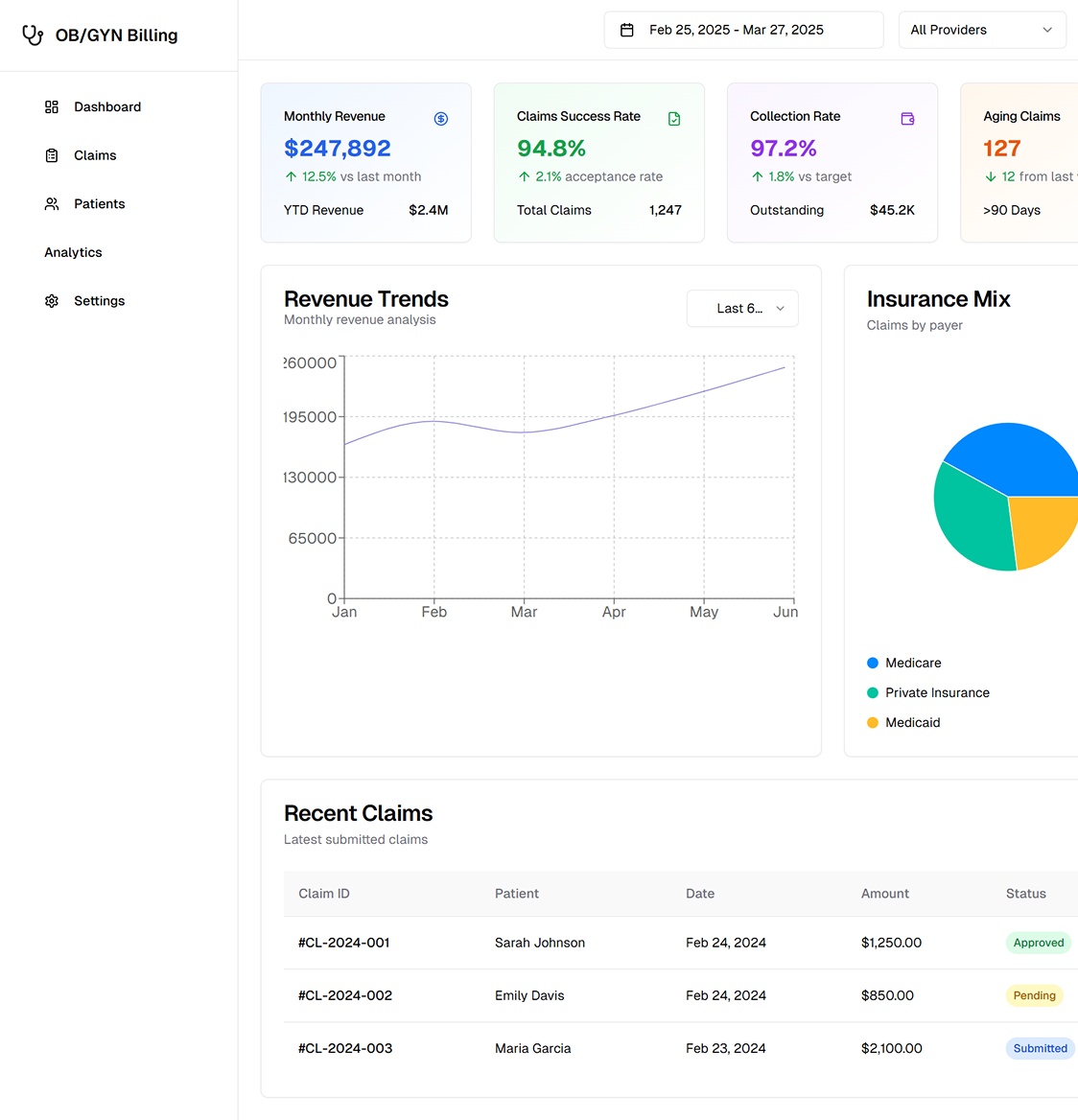
By verifying patient coverage upfront—be it private insurance, Medicaid, or Medicare—we prevent coverage gaps and incorrect submissions. Our system checks details like policy limits for family‐planning services and delivery codes, minimizing surprises down the line
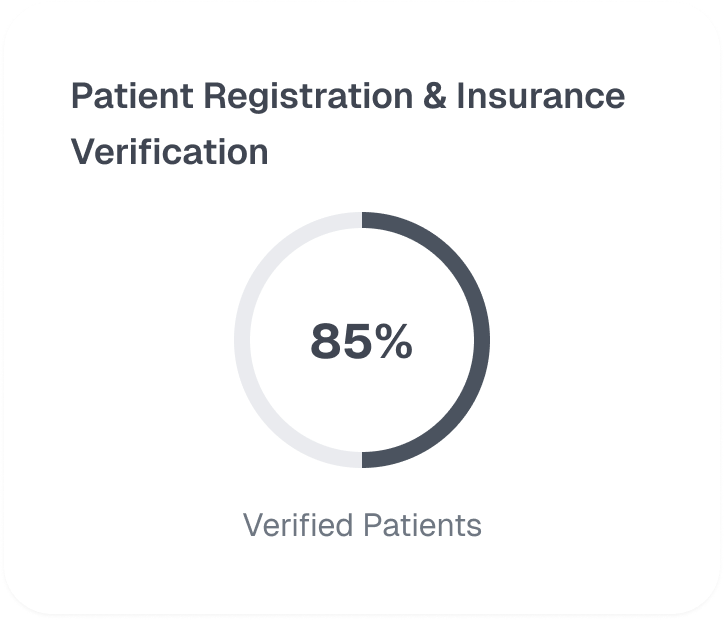
Correct CPT and ICD‐10 coding is crucial for OB/GYN procedures ranging from routine prenatal care to complex gynecologic surgeries. Our AAPC‐certified coders ensure each service—including anesthesia billing—is captured with the right modifiers and documentation, streamlining claim adjudication
Claims are submitted electronically for faster turnaround, with automated alerts for missing information or potential denials. Each submission is tracked in real time, allowing us to promptly correct errors and follow up on claims older than 18 days

Our proactive denial management approach identifies and addresses root causes—be it insufficient documentation, coding conflicts, or pre‐authorization lapses. We handle appeals swiftly, leveraging our knowledge of CMS and AMA guidelines to reverse denials and recover lost revenue

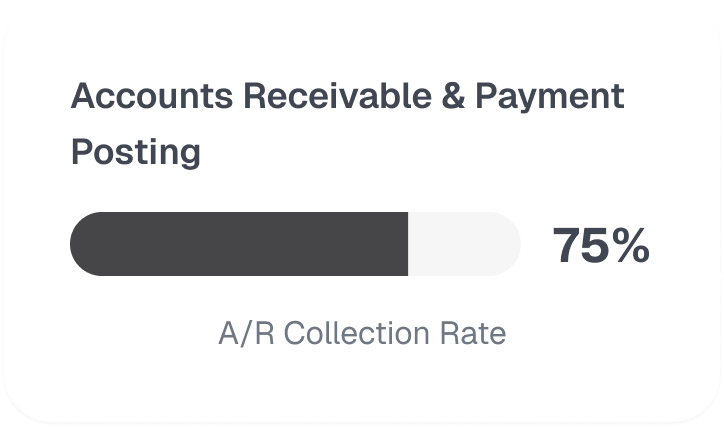
Timely payment posting ensures accurate financial records and clear patient statements. Our AR team monitors unpaid claims and outstanding balances, initiating follow‐ups and coordinating with insurers to expedite reimbursements. This systematic approach keeps your cash flow robust
Our RCM platform offers advanced analytics and detailed reporting—KPI dashboards, claim aging reports, and payer performance insights. Seamless integration with electronic health records (EHRs) ensures compliance with HIPAA and other regulatory standards, while real‐time data informs strategic decisions to continually improve practice profitability

.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers