BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Precision, Compliance, and Efficiency—All in One Comprehensive Ophthalmology RCM Solution
Schedule a CallRoutine Eye Exam Reimbursement Rate
Average Turnaround for Vision Plan Claims
Total Insurance & Patient Payments Collected
ASP-RCM Solutions offers specialized knowledge in CPT, ICD-10, and HCPCS coding for ophthalmology billing, ensuring accurate modifier usage, handling prior authorizations, and maintaining Medicare Part B rules, while minimizing rejections
We connect directly with your electronic medical records (EMR) system to capture charge data in real time. Our team validates charges against MUE (Medically Unlikely Edits), NCCI edits, and payer‐specific requirements, helping you avoid coding errors and reduce denials. By leveraging standards like HL7 or FHIR, we automate data transfer while maintaining top‐tier HIPAA compliance
Manual data entry can lead to costly mistakes. Our platform uses automated charge capture tools that pull essential details—such as diagnosis codes (ICD‐10) and procedure codes (CPT/HCPCS)—straight from your EMR. We then submit electronic claims via 837 files, track responses via 277 files, and reconcile 835 electronic remittances swiftly to keep your billing cycle moving efficiently
Ophthalmology often involves procedures requiring prior authorization (e.g., retinal surgeries, complex diagnostics). We facilitate real‐time eligibility checks through our integrated system, confirming patients’ coverage before services are rendered. This proactive approach helps prevent out‐of‐network surprises, underpayments, and delayed reimbursements—optimizing your practice’s cash flow
Our specialized claim scrubbing tool reviews each charge for correct code usage, modifier pairing (e.g., ‐54, ‐55, ‐56, when applicable), and compliance with CMS guidelines. By dealing with issues before claims reach the payer, we reduce denial rates and increase your clean claim submission percentage. Additionally, our software conducts thorough CCI (Correct Coding Initiative) checks to avoid bundling error
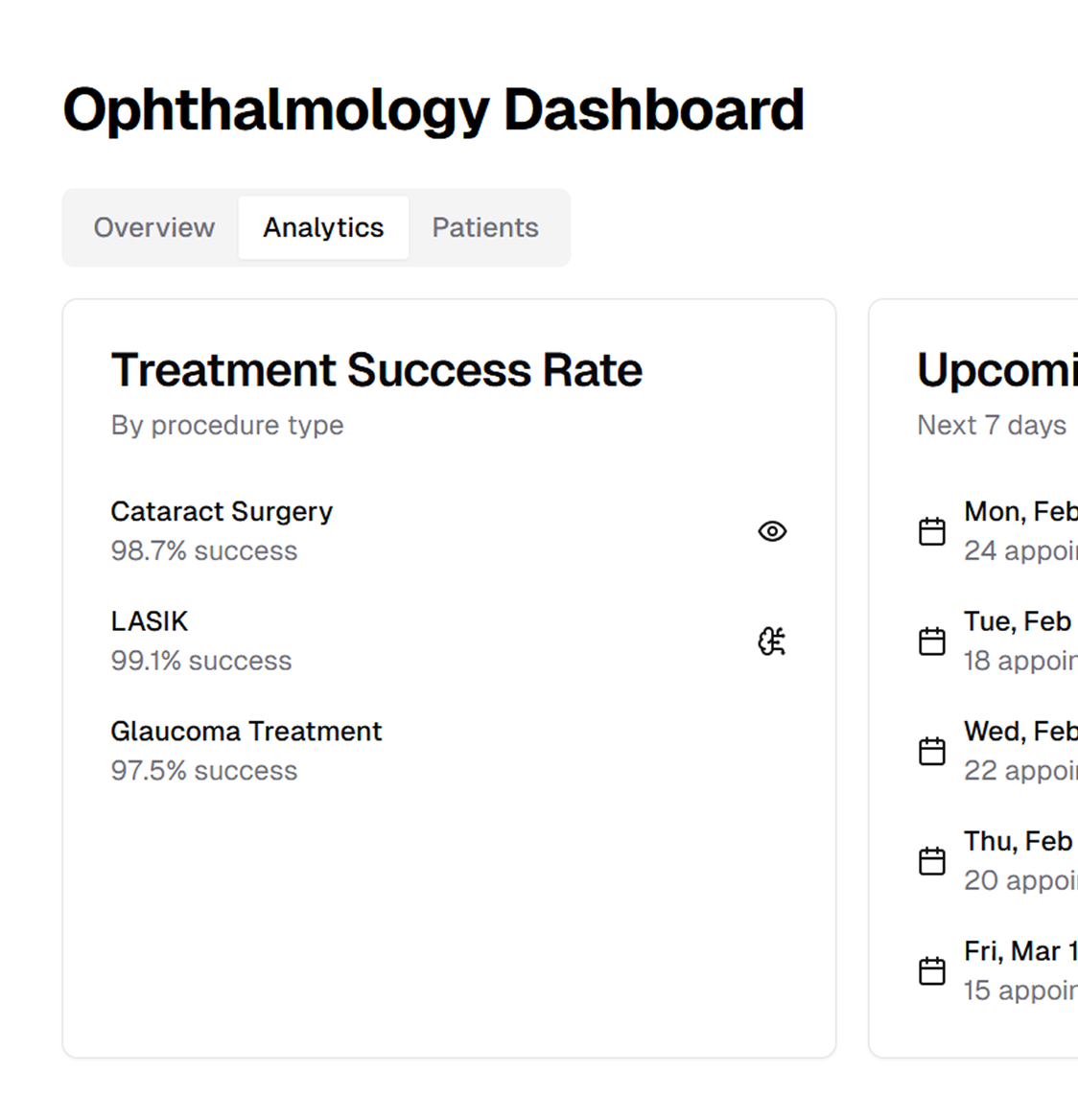
Your patients’ data security is paramount. We implement encrypted data transfers, multi‐factor authentication, and strict HIPAA and HITECH compliance to safeguard sensitive information. Meanwhile, our advanced dashboard analytics provide real‐time visibility into key performance indicators such as days in AR, clean claim rate, and reimbursement trends, helping you make informed decisions for sustainable growth
ASP‐RCM Solutions delivers an integrated suite of technical capabilities and RCM best practices tailored to the unique demands of ophthalmic care
We centralize patient demographics, verify insurance details, and assess benefits—often before the first appointment. This front‐end process, supported by real‐time EDI and eligibility tools, prevents denied claims and enables faster reimbursement
Our certified coders specialize in ophthalmology’s range of diagnostic and surgical services, from laser trabeculoplasty (CPT 65855) to vitrectomy (CPT 67036). By using ICD‐10 specificity (e.g., H40 series for glaucoma) and accurate modifiers (e.g., 59, 51, 50 for bilateral procedures), we ensure every claim meets payer requirements and captures full reimbursement potential
Our denial management team categorizes and reviews each rejection, focusing on root‐cause analysis—whether it’s a coding discrepancy, missing prior authorization, or incomplete documentation. We handle timely appeals, monitor short‐pay or no‐pay scenarios, and continuously improve processes to prevent recurrent errors
We stay current on CMS updates, including MIPS (Merit‐Based Incentive Payment System) and other quality measures pertinent to ophthalmology. Our billing workflows incorporate 5010 transaction standards and regularly updated payer policies to maintain continuous compliance and avoid penalties
Harness the power of real‐time dashboards to gain actionable insights into your practice’s financial health. We provide metrics like lag days, collection ratios, and revenue per encounter, enabling data‐driven decisions on contract negotiations, resource allocation, and growth strategies
Whether your ophthalmology practice is a solo clinic or a multi‐location network, our solution scales your needs. We offer 24/7 remote support, handle peak workloads, and seamlessly adapt to your existing EMR/PM systems. By automating routine tasks and leveraging our specialized team, you get consistent results without the overhead of in‐house billing complexities
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers