BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Inconsistencies in eligibility verification and benefits checks will lead to insurance denials, delayed reimbursements, and revenue loss to a practice
Schedule a CallResponse Time
Accuracy Rate
Verifications Completed
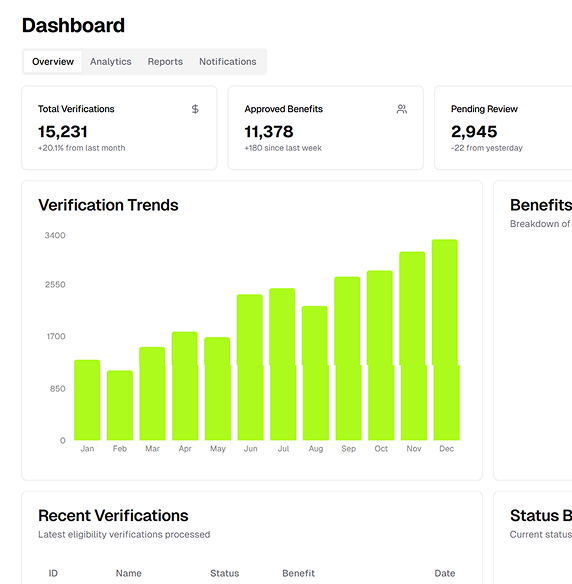
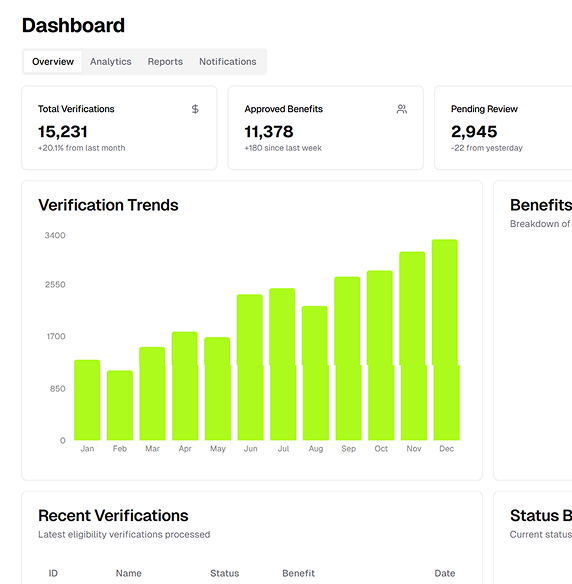
We take a data-driven approach to eligibility verification that prioritizes efficiency, accuracy, and compliance. Here’s why healthcare providers and patients trust us
Our system provides granular details such as CPT code-specific benefits, authorization requirements, and cost-sharing details, enabling informed decisions.
By automating manual verification processes, we minimize errors and reduce turnaround times, enabling instant confirmation of patient eligibility.
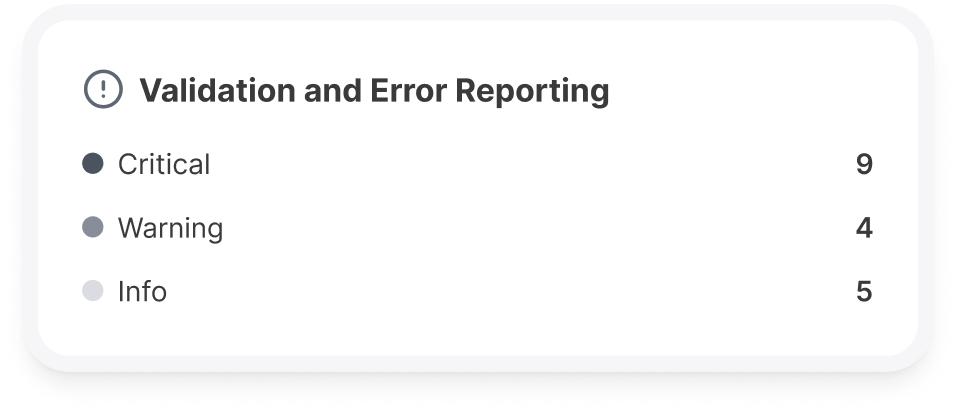
Proprietary algorithms flag discrepancies in payer responses, ensuring you never miss critical coverage details.
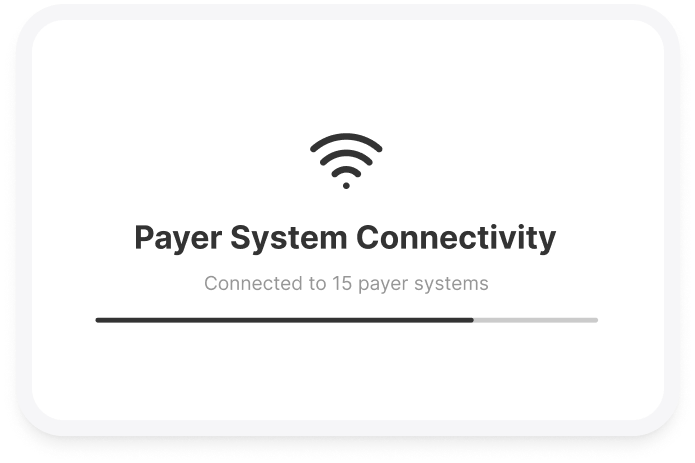
Our platform connects directly to hundreds of payer databases via EDI (Electronic Data Interchange), ensuring real-time updates on coverage.
We adhere to HIPAA and other regulatory standards, ensuring secure handling of sensitive patient data while maintaining operational excellence
Our eligibility verification and benefits check process are designed with healthcare providers and RCM professionals in mind. Here's how we achieve operational excellence
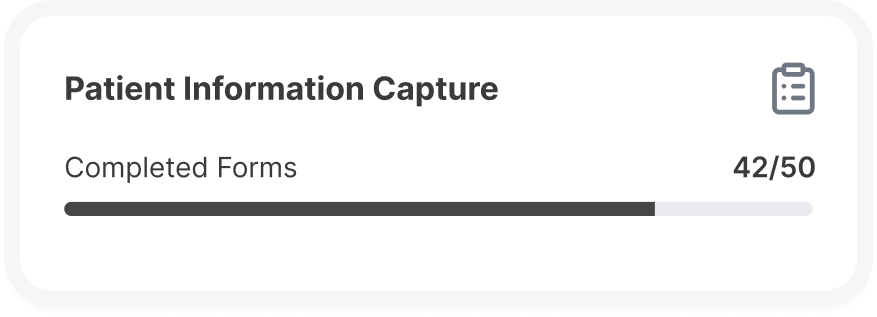
Through seamless integration with your EMR/EHR systems, we automatically capture patient demographics and insurance details at the point of scheduling.
Our platform establishes direct connections with payer systems, ensuring real-time eligibility status for Medicare, Medicaid, and commercial insurers
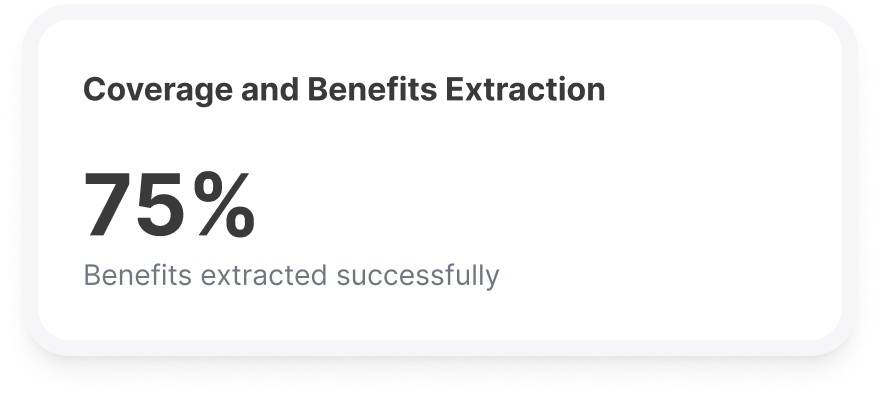
Beyond basic eligibility, we pull data on co-pays, deductibles, out-of-pocket limits, and specific coverage for planned procedures or services.
Advanced rule engines validate payer responses, highlighting missing or inaccurate data for proactive resolution
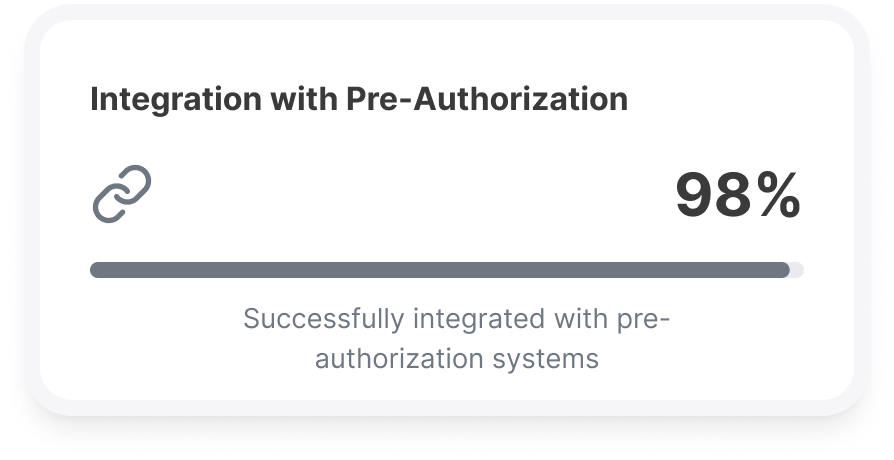
If a procedure requires prior authorization, our system identifies this need, integrating with pre-authorization workflows to streamline approvals.
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers