BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Secure Records. Sharper Insights. Stronger Reimbursement.
Schedule a CallEfficient Rate
Processing Time
Accuracy Rate
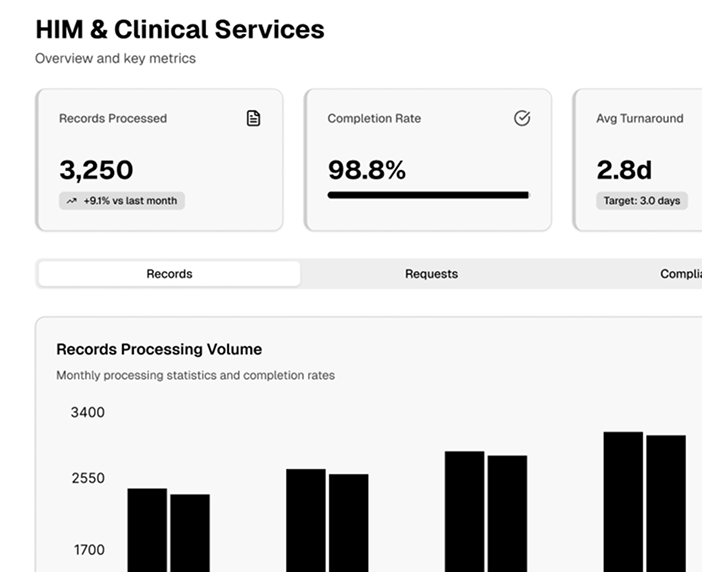
Certified HIM professionals, clinical documentation specialists, and credentialed coders collaborate to ensure data accuracy, comply with federal mandates, and improve provider performance.
We sit shoulder-to-shoulder with providers, translating clinical language into precise, compliant codes that protect Case-Mix Index, MS-DRG accuracy, and quality scores—without tech distractions.
End-to-end record capture, indexing, retention, and privacy audits keep PHI locked tight and surveyors off your back.
Fast, rule-tight disclosures for payers, attorneys, and auditors, backed by defensible policies and iron-clad audit trails.
We roll up clean, validated data for HEDIS, MIPS, ACO, and core measures so leadership gets actionable quality insights—based on human review, not automated guesswork.
Prospective chart reviews flag coding gaps, medical-necessity issues, and modifier misfires before claims ever leave the building.
We embed ourselves in your workflows, straighten out messy documentation, and turn incomplete records into audit-proof revenue generators—all without slowing clinicians down.
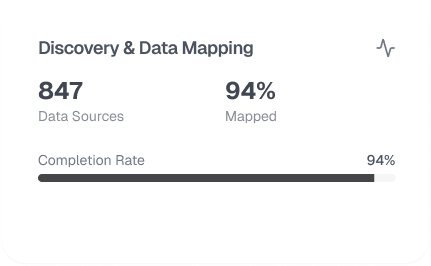
We tap into Epic, Cerner, Meditech, or your home-grown EMR, mapping every data touchpoint and locating weak links.
Credentialed coders manually validate ICD-10-CM/PCS, CPT, and HCPCS codes against physician notes and 2025 CMS rules.
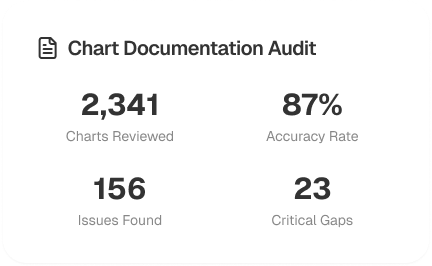
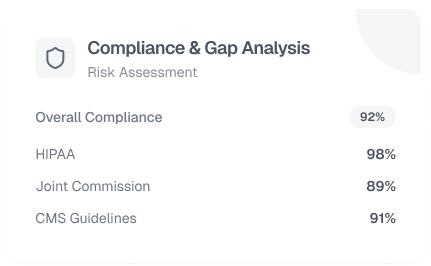
Findings are cross-checked with CMS, OIG, MAC, and HIPAA requirements—no shortcuts.
You get a prioritized playbook: quick wins, long-term fixes, forecasted revenue impact.

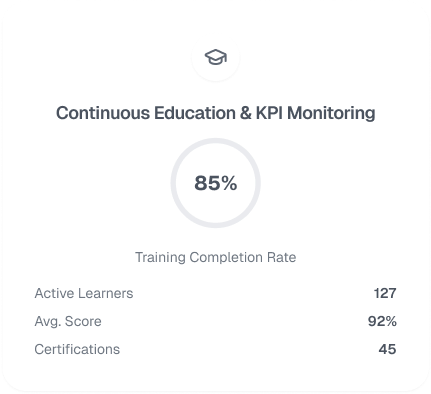
Monthly sampling, 1:1 physician coaching, and old-school spreadsheets keep gains locked in.
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers