BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Precision Documentation for Optimized Revenue and Compliance
Schedule a CallQueries Answered
Within
DRG match
 1.png)
 1.png)
Strong documentation drives care quality, proper reimbursement, and compliance with evolving value-based care standards.
We ensure medical records reflect accurate diagnoses and coding, securing appropriate reimbursement and enhancing care outcomes.
We help clients meet documentation standards for risk adjustment and quality scoring under value-based payment models.
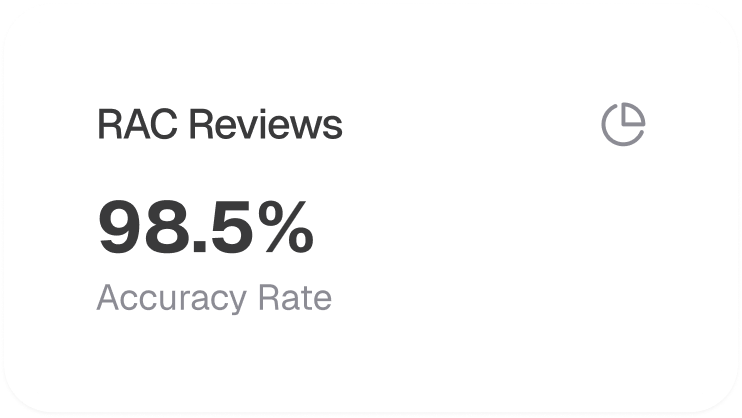
Supports medical necessity Ensures proper DRG/HCC assignment Enhances audit preparedness (e.g., RAC audits)
Higher quality scores and reporting accuracy Better alignment between documentation and billing Increased compliance and revenue capture
Interdisciplinary engagement with physicians, coders, and staff ensures consistent documentation quality and regulatory agility.
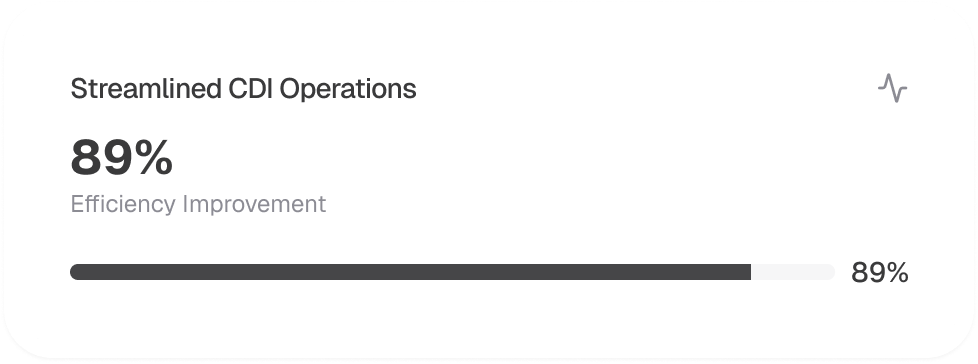
From multi-specialty coding to scalable solutions, we ensure streamlined processes and measurable results
Real-time coding feedback pre-discharge
Confirming SOI and ROM accuracy

Clarifying documentation while maintaining integrity

Root cause analysis and mitigation strategies
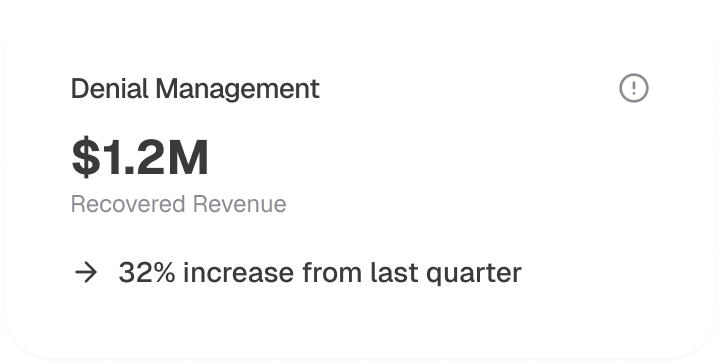
Proactive documentation checks and appeals support
Data analytics and workflow tools ensure adaptability and performance tracking

.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers