BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Dedicated to Delivering High-Quality Risk Adjustment Coding
Schedule a CallAudit-grade HCCs
Prior-Year Recapture Rate
RADV Disallowance Rate
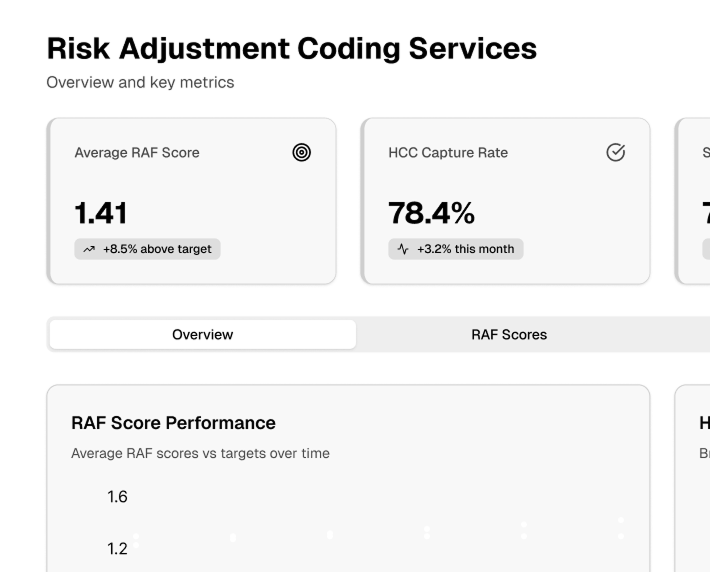
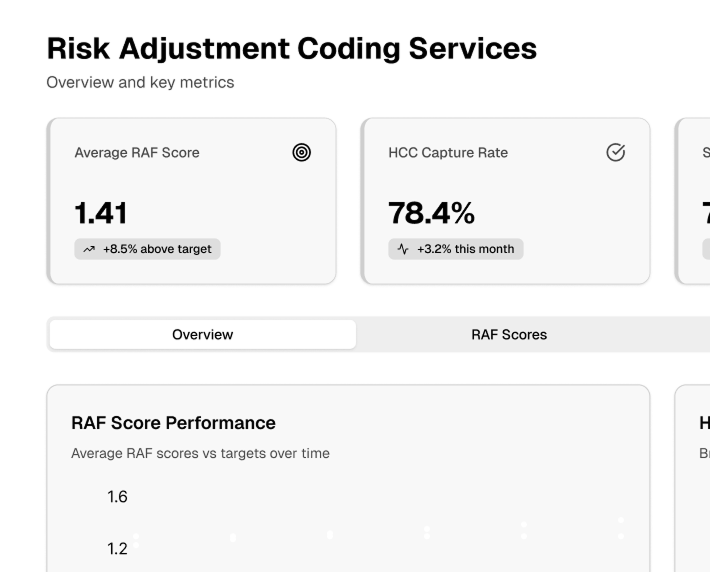
From prospective and concurrent reviews to targeted chart evaluations and advanced validation processes, each method plays a crucial role in improving coding accuracy and aligning with regulatory requirements
Our certified coding specialists focus on HCC coding, precisely recording patient conditions to represent their actual health status and risk ratings.
We thoroughly evaluate patient charts and data to identify missing or inaccurate diagnoses.
We employ cutting-edge workflow management technologies to expedite turnaround times, increase efficiency, and simplify coding
We employ cutting-edge workflow management technologies to expedite turnaround times, increase efficiency, and simplify coding
We provide in-depth data and analytics to help you comprehensively understand your risk adjustment performance
This heading reflects the full scope of services, emphasizing the focus on accuracy, compliance, and optimization of risk adjustment and coding processes. It is professional, clear, and aligns with the audience's expectations in the healthcare domain
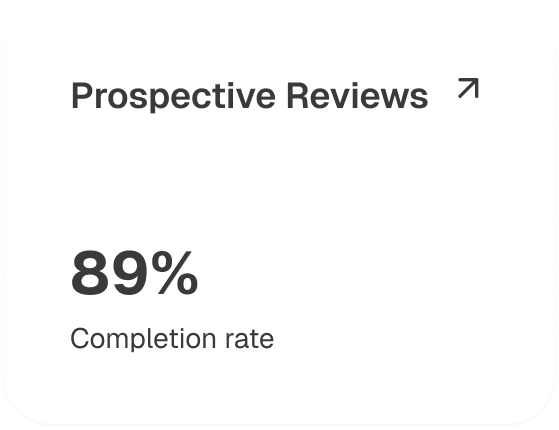
Prospective reviews, conducted before patient encounters, help identify patients with potential risk adjustment opportunities
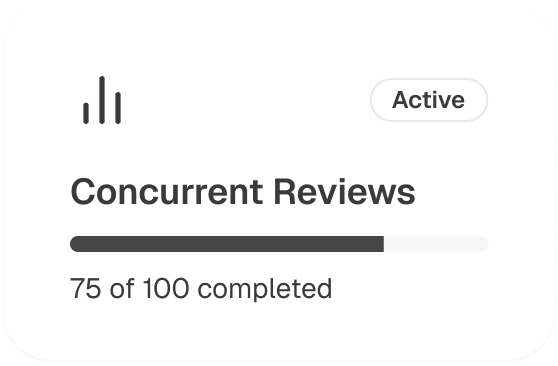
Concurrent reviews help ensure that all relevant diagnoses are documented and coded accurately at the point of care, reducing the need for retrospective corrections
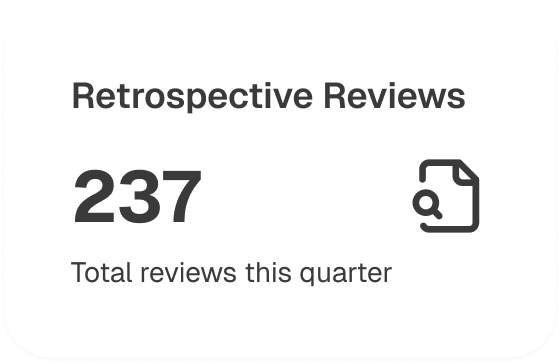
Retrospective reviews are carried out after patient encounters. They involve analyzing past medical records to identify missing or incorrect codes
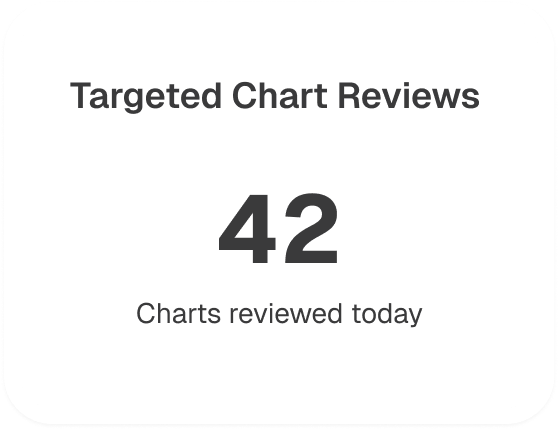
Targeted chart reviews focus on high-risk patients or those with complex medical histories and aim to identify specific coding opportunities
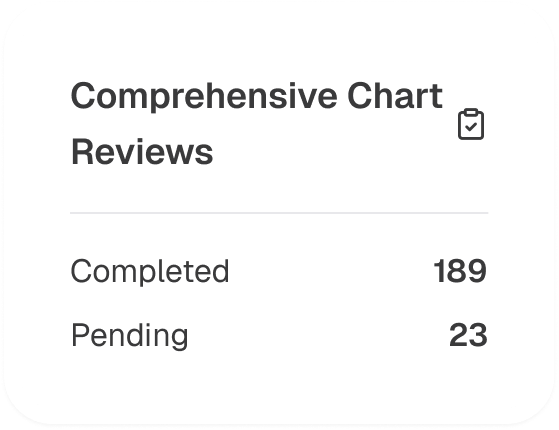
Thorough reviews of a patient’s medical record are needed to ensure that all relevant diagnoses are accurately documented and coded
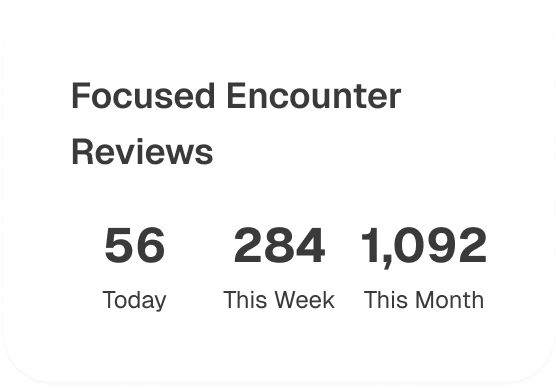
Reviews centered around specific patient encounters (e.g., annual wellness visits, hospital admissions) where coding opportunities may be more prevalent
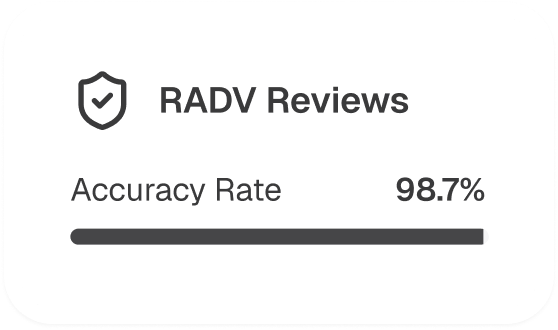
RADV reviews help identify discrepancies and mitigate compliance risks
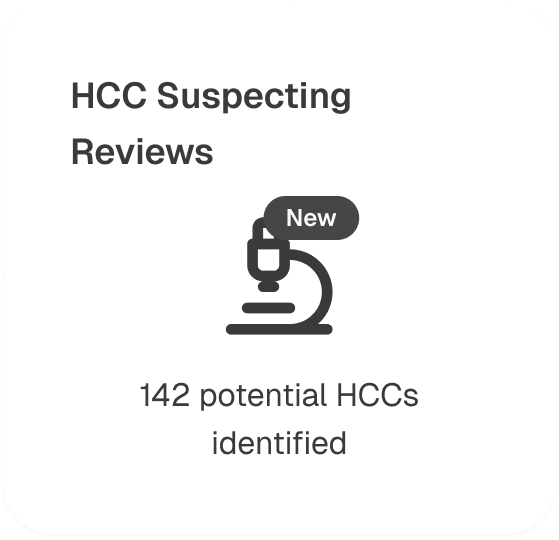
Utilizing advanced analytics and machine learning algorithms, HCC suspecting reviews help identify potential diagnoses that may not have been documented based on patient clinical data patterns
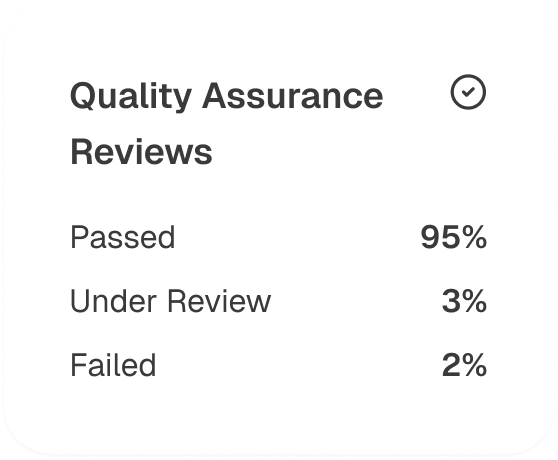
A final layer of review to ensure that all coding practices adhere to internal quality standards and regulatory requirements
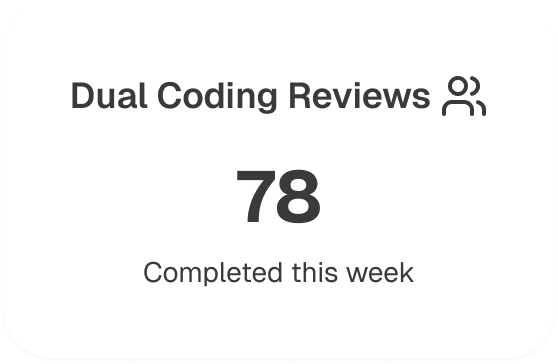
Conducted to compare coding results from two separate coders or teams to ensure consistency and accuracy
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers