BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
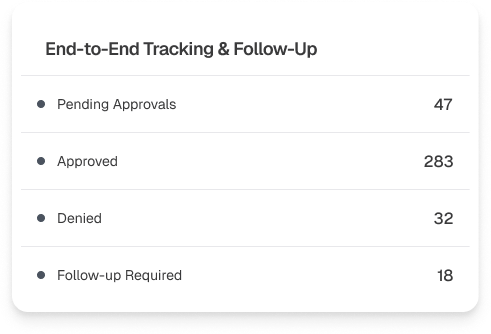
We strive to create a seamless and hassle-free process for healthcare providers and patients, ensuring timely approvals and minimizing patient care delays
Schedule a CallTurnaround Time
Success Rate
Requests Handled
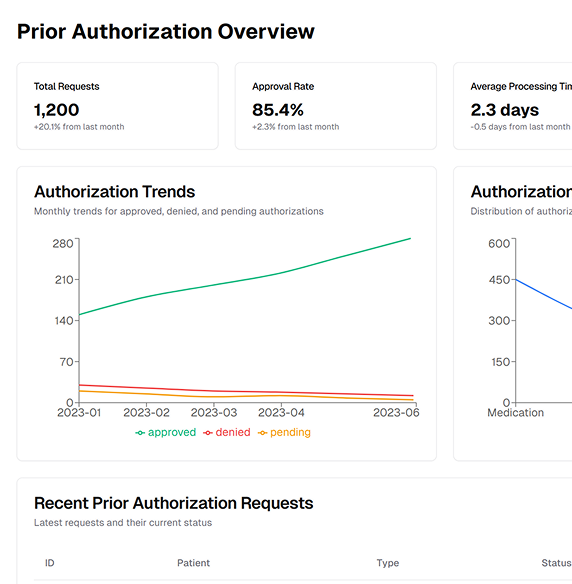
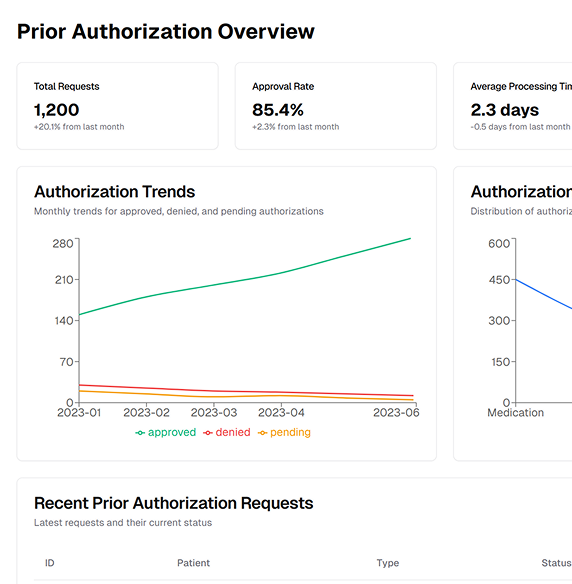
Prior authorization is crucial in the healthcare industry. It is the foundation of a practice’s revenue cycle and is required for healthcare services
To speed up authorization procedures, our knowledgeable staff cultivates connections and is aware of insurers' subtleties
Workflows are streamlined by automation in eligibility verification and prior authorization submissions, such as patient data that is automatically filled in
We can determine and verify the medical necessity necessary for a prior authorization to be deemed effective
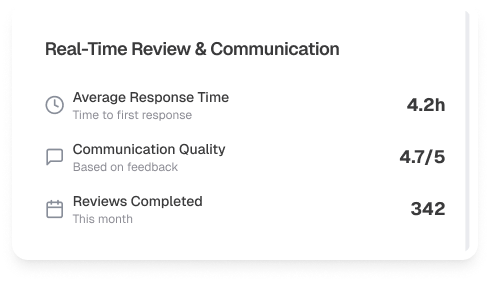
Using specialist software, we closely monitor and follow up on requests for eligibility and prior permission to maintain regular contact with insurers
By directing medical professionals toward therapies and drugs with a higher chance of insurance acceptance, analytics tools can save time and money
Our expert prior authorization services streamline the approval process so you can focus on delivering exceptional care, not chasing paperwork
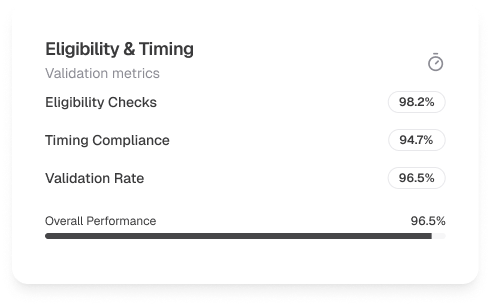
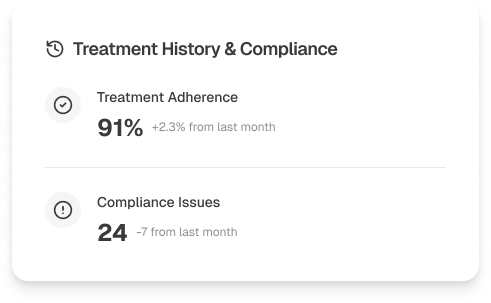
To avoid delays or denials, we ensure the appointment falls within the approved authorization date range and meets any payer-specific visit requirements
Our team submits precise CPT, HCPCS, and diagnosis codes that align with payer medical necessity criteria. All codes and clinical notes are thoroughly documented to support the request
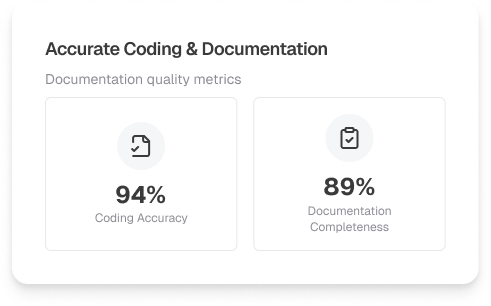
We verify if the requested services meet appropriate levels of care and are backed by a well-documented Plan of Care. When necessary, MRIs, psychological evaluations, and other clinical elements are included
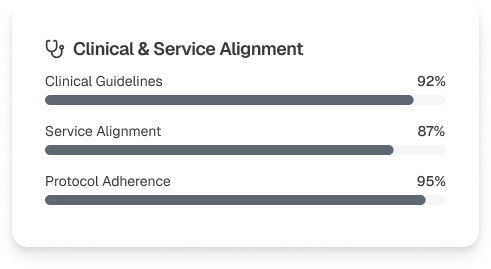
Where applicable, we confirm that conservative treatments or therapies have been attempted and documented, meeting payer prerequisites for advanced care approvals
Our team keeps close contact with payers and providers, initiating Peer-to-Peer reviews to support medical necessity and ensure timely decision-making
From submission to approval, we monitor every step, addressing payer requests and minimizing turnaround time to keep your operations and patient care moving smoothly
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers