BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Comprehensive ABA Billing Services, with accurate claims submission, seamless documentation, timely authorization follow-up and consistent revenue flow
Schedule a CallTotal Claims Billed
Claim Approval Rate
Denial Rate
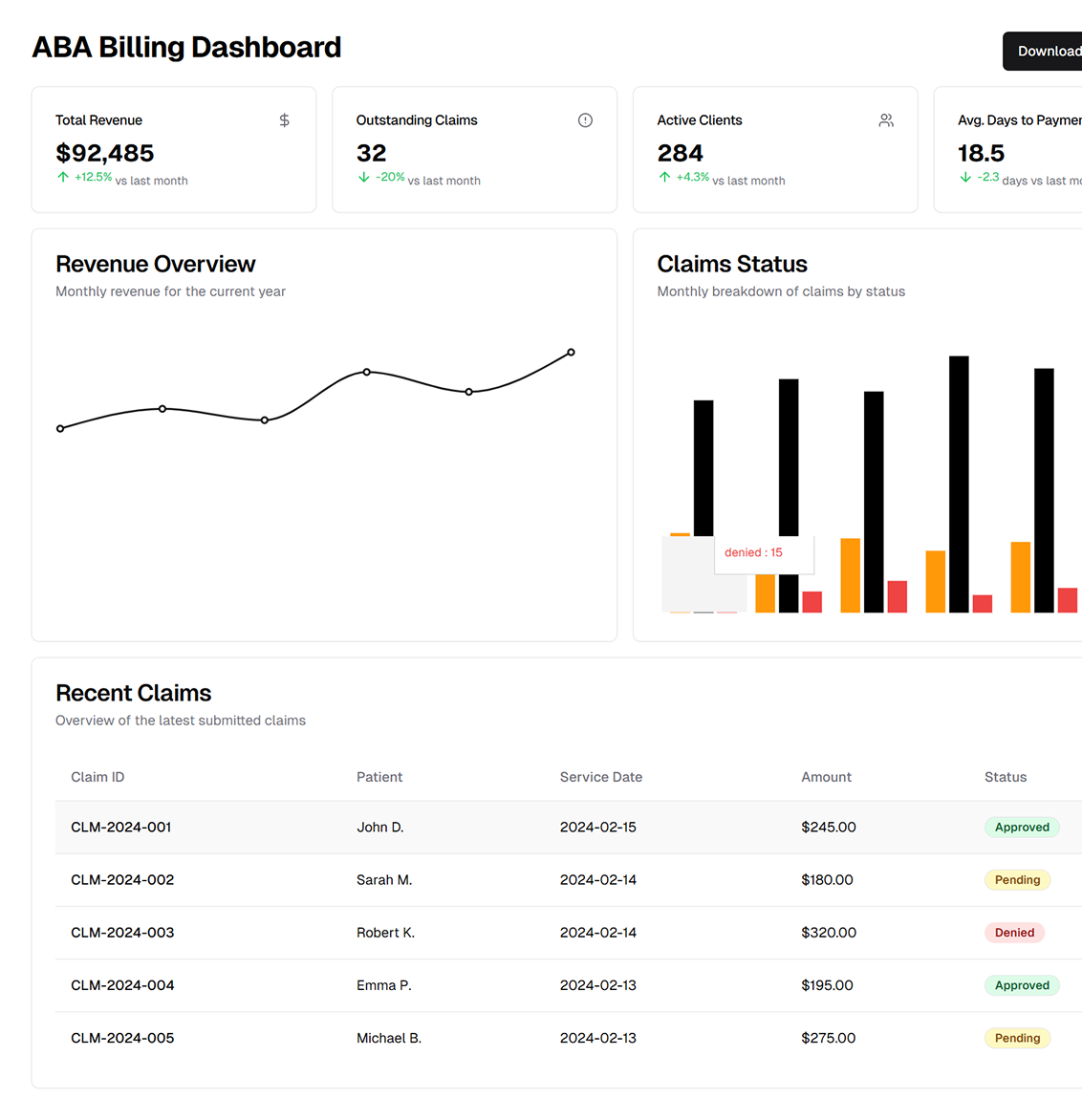
ASP-RCM Solutions provides customized billing services for ABA therapy practices. It ensures compliance with payer policies and Medicaid updates, simplifies billing processes, and optimizes reimbursements
Our team stays updated with changing payer policies, fee schedules, and reimbursement guidelines to ensure your claims are accurate and timely. This reduces rejections and expedites the revenue cycle
We manage Medicaid requirements, copays, and deductibles for private insurance plans, ensuring compliance and helping you maximize revenue potential while staying current with market trends
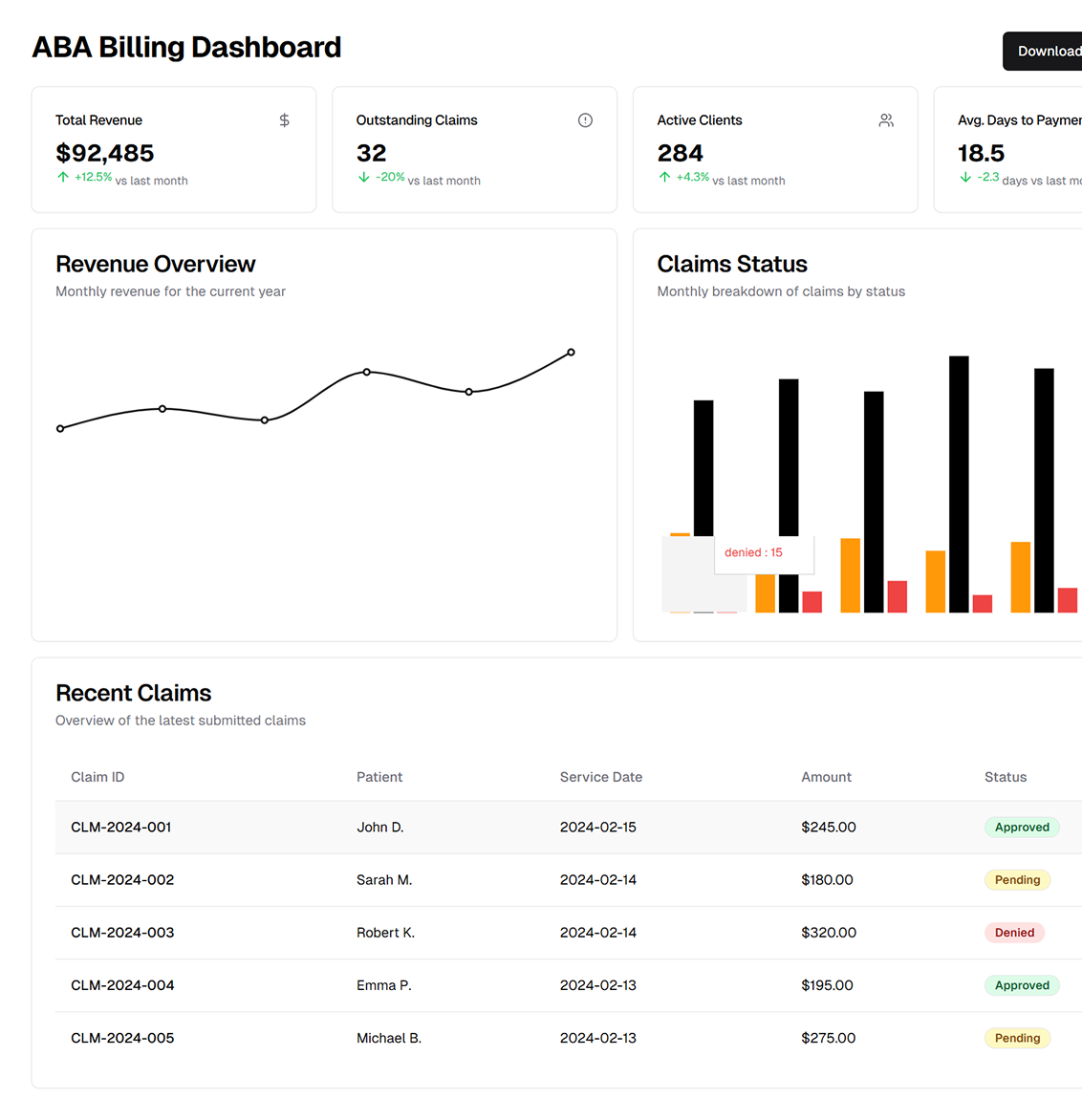
By implementing efficient pre-billing, post-billing, and follow-up processes, we streamline the entire revenue cycle, from patient intake to payment reconciliation.
Our proprietary solutions adapt to the unique requirements of ABA therapy practices, addressing challenges like documentation gaps, denial resolutions, and accurate code assignments
Through dedicated billing assistance, ASP-RCM enables ABA practitioners to invest time in improving patient outcomes, leaving the financial complexities to our expert team
Understanding and Tackling ABA Billing Complexities
Our pre-billing operations include patient data collection, insurance benefit verification, and prior authorization submissions ensuring all prerequisites are met before treatment begins, minimizing delays
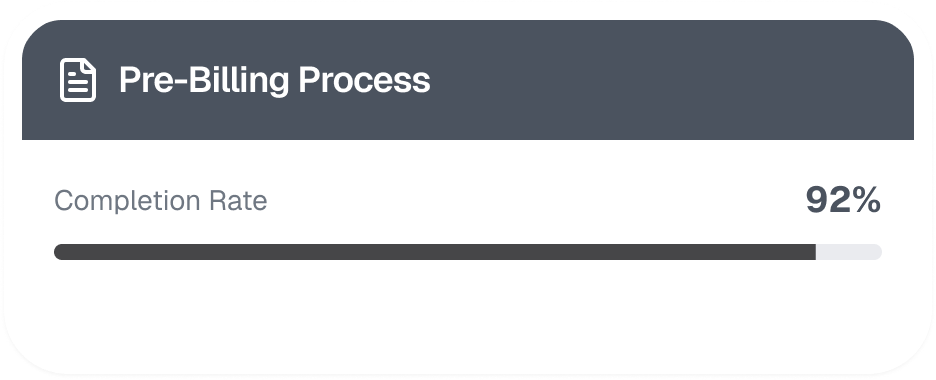
Accurate claims submission is achieved by adhering to CPT and HCPCS codes specific to ABA therapy. Documentation verification and proper use of modifiers ensure reimbursement accuracy and reduce claim rejections
We analyze claim denials, identify root causes, and resubmit corrected claims promptly. Additionally, our team manages the appeals process to secure appropriate compensation for underpaid or denied claims
Advanced billing software and EHR systems streamline workflows, automate repetitive tasks, and reduce manual errors. These scalable solutions adapt to the growth needs of your practice
Our team conducts regular audits to ensure adherence to federal and state regulations. We monitor payer guideline changes proactively and assist with external audits, ensuring transparency and compliance
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers