BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
Precision that powers your revenue. Experience the power of proactive revenue cycle management that keeps your healthcare organization ahead, efficient, and thriving.
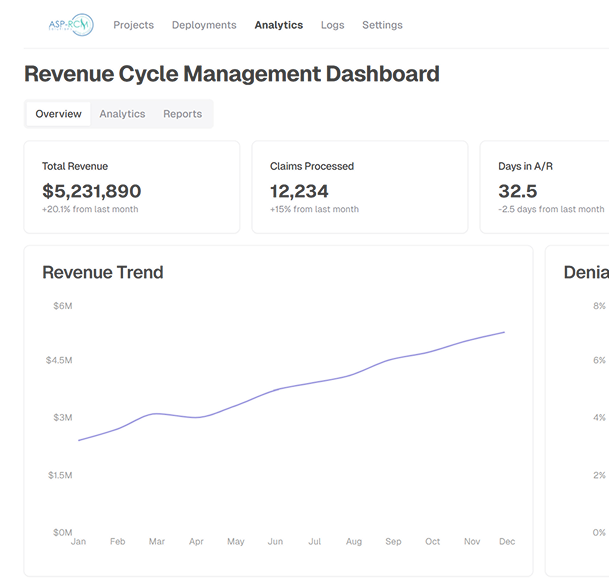
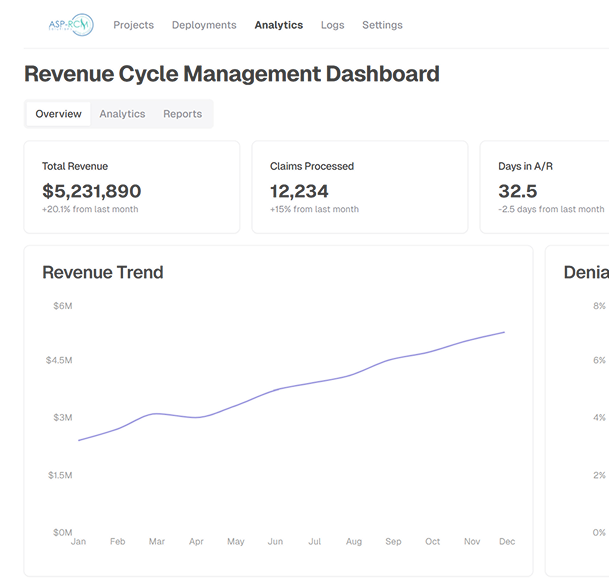
Schedule a CallClaim Acceptance Rate
Average Days to Payment
Denial Rate
We offer end-to-end medical billing, coding, and accounts receivable management services designed to streamline complex administrative and clinical workflows, allowing you to focus on patient care.
ASP-RCM Revenue Cycle services are geared to meet a wide range of concerns and challenges faced by hospitals and physicians while increasing cash flow
We optimize each stage of the revenue cycle from patient intake and coding to billing and collections, ensuring faster reimbursements, fewer errors, and improved financial performance.
Using Lean Six Sigma best practices, we refine workflows and enhance operational efficiency to achieve optimal ASP-RCM performance
Our "divide and rule" approach streamlines workflows by dividing tasks into modules, ensuring efficient job allocation and reducing administrative overhead
We take a strategic approach to A/R days, applying proven methods and streamlining practice operations to speed up collections and cut down aging.
ASP-RCM offers healthcare providers a robust, scalable solution to navigate the complexities of modern revenue cycle management
.jpg)
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers
BLOG • Jan 22, 2026
Medicare 2026: Essential Coverage Changes for Seniors and Healthcare Providers